Heart and the Vagus Nerve Connection
The vagus nerve, a key component of the parasympathetic nervous system, plays a significant role in regulating heart rate and blood pressure. Autonomic imbalance, often resulting from damage to the vagus nerve, causes increased sympathetic nerve activity. This increased activity is not just a reaction mechanism, but can also cause diastolic dysfunction, increase the risk of heart attack and weaken blood vessels, and potentially influence the development of other heart diseases. Decreased vagal functionality can be linked to several factors, such as infections, chronic diseases and age-related inflammation associated (doi: 10.1007/s11357-022-00616-1), and contribute to:
Impaired Vagal Tone
Reduced vagal tone, often observed during ageing and various diseases, directly affects the functioning of the vagus nerve. This reduction in vagal tone adversely affects the "rest and digest" response, causing a noticeable reduction in heart rate variability (HRV), an important indicator of the health of both the heart and the autonomic nervous system. Lower HRV indicates a reduced adaptability and resistance of the cardiac system and an increased risk of cardiovascular disease doi: 10.1161/CIRCULATIONAHA.113.005361).
Cardiac Rhythm Disruption
A weakened vagal tone, a common consequence of vagus nerve impairment, can also lead to insufficient modulation of heart rate. This can result in an erratic heart rate, either too fast or too slow, and a lack of stability in heart rate control. Without the stabilising influence of the vagus nerve, the heart becomes more vulnerable to rhythm disturbances, such as tachycardia or bradycardia (doi: 10.1080/17434440.2019.1643234).
Vascular Deterioration
Damage to the vagus nerve can significantly worsen cardiovascular deterioration by contributing to endothelial dysfunction. A reduction in vagal tone negatively impacts the endothelium, diminishing its capacity to effectively regulate vascular tone and blood flow. This endothelial dysfunction may manifest as reduced flow-mediated dilation. Such dysfunction not only increases the risk of atherosclerosis but also aggravates conditions in individuals with heart failure (doi: 10.3389/fcvm.2022.866957).
Impact on Inflammatory Response
Impaired vagal function can exacerbate heart failure and increase the risk of other heart diseases, primarily by disrupting anti-inflammatory pathways. The vagus nerve plays a key role in regulating heart function and modulating inflammation. In heart failure, especially with preserved ejection fraction (HFpEF), reduced vagal tone may lead to increased inflammation, contributing to the progression of fibrosis and deterioration of cardiac function (doi: 10.1161/JAHA.121.023582).
Impaired ventricular function
The vagus nerve plays a pivotal role in autonomously regulating heart rate and contractility. This regulation can be quantified using a medical parameter called global longitudinal strain (GLS), which measures the percentage of deformation in the heart muscle during its contraction. Damage to the vagus nerve can impair ventricular function, often contributing to cardiovascular complications such as heart failure, myocardial infarction, or cardiomyopathy. This deterioration can result in decreased pumping ability, reduced cardiac output, and impaired circulation. In diabetic and metabolic syndrome patients, GLS can be used to detect early changes in cardiac function, even before other clinical symptoms appear (doi: 10.1007/s12265-018-9853-6).
Cardiac Remodelling
The vagus nerve is responsible for the autonomic regulation of heart rate and contractility, dependent on the parasympathetic branch. Stressors can damage the vagus nerve, which can lead to impaired ventricular function, often contributing to cardiovascular complications such as heart failure, myocardial infarction, or cardiomyopathy. This deterioration may result in decreased pumping capacity, decreased cardiac output, and circulatory dysfunction (doi: 10.1161/JAHA.121.023582; doi: 10.1007/s10741-010-9190-6).
Enhanced Heart Rate Variability (HRV)
Neuromodulation with Nurosym enhances the activity of the parasympathetic nervous system, thereby improving the heart rate variability (HRV) index. HRV is a marker of cardiac and autonomic health and tends to decline with age, which increases the risk of cardiovascular mortality. Improved HRV indicates a more resilient and adaptive cardiovascular system, capable of effectively coping with stressors. Additionally, Nurosym's neuromodulation may counteract the excessive sympathetic activity often observed in conditions of reduced vagal tone (doi: 10.1016/j.jacep.2020.02.014, doi: 10.1161/CIRCULATIONAHA.113.005361).
Cardiac Rhythm Regulation
Nurosym has been shown to reduce arrhythmias and stabilise cardiac electrophysiological properties, such as prolonging the effective refractory period (ERP) and reducing ERP dispersion. The antiarrhythmic effects of Nurosym are attributed to its antiadrenergic effects and is thought to be mediated by increasing vagal tone, indicated by reducing levels of neuropeptide Y (NPY) and other cytokines associated with inflammation. Additionally, Nurosym may not only lead to improved heart rate regulation but also stabilise the heart rate and prevent in progression of arrhythmias. This is particularly important in the context of conditions such as atrial and ventricular fibrillation (doi: 10.1161/JAHA.121.023582, doi: 10.1016/j.jacep.2020.08.025).
Cardiovascular Function Enhancement
Nurosym positively influences the function of macrovascular endothelium in patients with heart failure and reduced ejection fraction (HFrEF). One hour of Nurosym neuromodulation led to enhanced flow-mediated dilation (FMD), as determined by brachial artery reactivity testing, indicating improved function of larger blood vessels. This trend is associated with the advancement of microvascular endothelial function, crucial for the formation of the inner lining of blood vessels. Such progress may be beneficial in mitigating cardiovascular and hypertension deterioration (doi: 10.1016/j.cardfail.2022.10.278, doi: 10.1016/j.cardfail.2020.12.017).
Reduction of Inflammatory Markers
Nurosym, by reducing inflammation (TNF-α, CRP) levels, benefits heart function in patients with heart failure with preserved ejection fraction (HFpEF) and significantly decreases atrial fibrillation (AF) burden. Its mechanism of action involves neural circuits that regulate immunity through the inflammatory reflex, a prototypical reflex circuit that maintains immunological homeostasis. This reflex is a key mediator in the anti-inflammatory pathway. This pathway is crucial in addressing oxidative stress and cellular metabolism, both significant factors in HFpEF pathophysiology (doi: 10.1007/s10286-023-00997-z, doi: 10.1016/j.cardfail.2022.10.278).
Ventricular function improvement
Nurosym has been shown to reduce diastolic dysfunction which often leads to heart failure with preserved ejection fraction (HFpEF) in patients with atrial fibrillation (AF). This improvement is reflected in the enhanced function of the left ventricle as indicated by reduction of cardiac global longitudinal strain (GLS) and it is the indicator of better heart function. This effect preserves cardiac function and reduces risk factors associated with ischemic stroke, heart failure, cardiomyopathy, and cardiac fibrosis (doi: 10.1161/JAHA.121.023582, doi: 10.1007/s12265-018-9853-6).
Reduced Harmful Cardiac Remodelling
In heart failure and various heart diseases such as atrial fibrillation or ischemia-induced ventricular arrhythmia, the heart undergoes structural changes - a process called remodelling - which can be harmful. Nurosym has been shown to reduce the burden of atrial fibrillation by potentially preventing or slowing this harmful remodelling process. This is particularly important in the atria, which are susceptible to enlargement and reduced performance due to persistent atrial fibrillation (doi: 10.1080/17434440.2019.1643234, 10.1161/JAHA.120.020865).
Nurosym Research-Based Evidence
92% of Nurosym patients after 3 months of regular treatment observe positive outcomes in heart rate variability (HRV), which is an indicator of an enhancement of the parasympathetic nervous system response.
In the Nurosym research, the neuromodulation group was associated with improved heart rate variability (HRV), including a substantial 61% increase in measures of cardiac vagal activity (HF parameter, important in respiratory sinus arrhythmia), along with significant improvements in other parameters (18% RMSSD, 25% pRR50, 14% SDRR), when compared to the placebo group (doi: 10.1371/journal.pone.0263833).
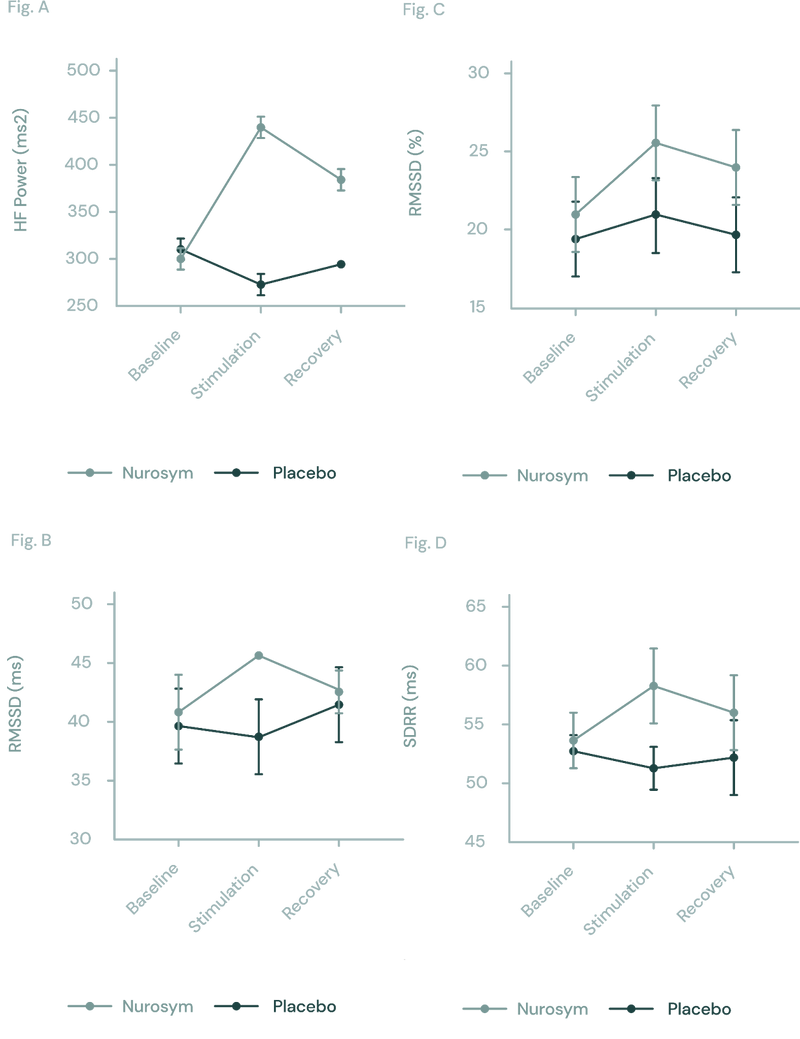
Fig (A, B, C D). The response of autonomic function measured by HRV in Nurosym or Placebo conditions over time: (A) HF, (B) RMSSD, (C) pRR50, (D) SDRR. With Nurosym, the measurements of HF, RMSSD, PRR50 and SDRR were significantly higher than those in Placebo (Parasym Clinical Trials, doi: 10.1371/journal.pone.0263833).
These findings suggest a notable shift towards the parasympathetic side, indicating a more pronounced relaxation response during Nurosym neuromodulation (doi: 10.1161/JAHA.121.023582).
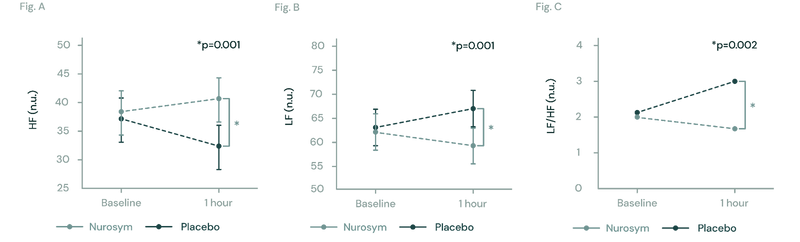
Fig (A, B, C). The figures illustrate changes in heart rate variability (HRV) during Nurosym neuromodulation. In Figure (A), High Frequency HRV significantly increases (*p=0.001). In Figure (B), Low Frequency HRV significantly decreases (*P=0.001). Figure (C) demonstrates that the ratio of LF to HF is significantly decreased (*p=0.002) (Parasym Clinical Trials, doi: 10.1371/journal.pone.0263833).
86% of Nurosym tachycardia patients reported reduced heart palpitations over 2 months of treatment without significant adverse effects. In Nurosym research, according to ΔHR analyses that revealed an ~40% improvement (doi: 10.1016/j.hrthm.2023.04.051)
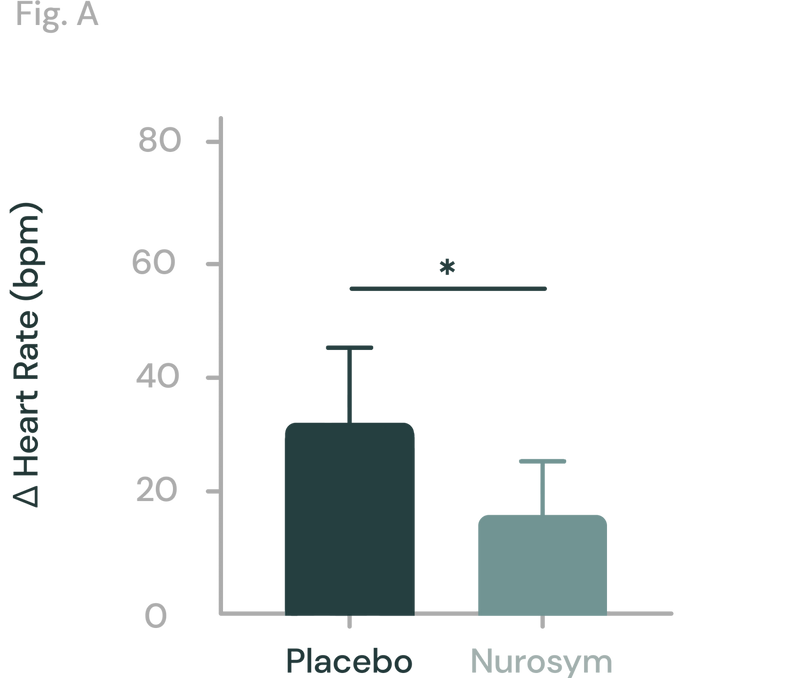
Fig. Effect of Nurosym neuromodulation vs. Placebo control on the postural change in heart rate [Δ (heart rate)] at 2 months (Parasym Clinical Trials, doi: 10.1016/j.hrthm.2023.04.051).
After just one day of Nurosym therapy, there was a remarkable 50% increase in blood vessel flow-mediated dilatation, which signifies healthy vascular function. (doi: 10.1016/j.cardfail.2020.12.017).
Nurosym research also has shown a positive effect on peripheral microcirculation, as indicated by increased blood perfusion (during LSCI imaging) (doi: 10.1016/j.cardfail.2020.12.017).
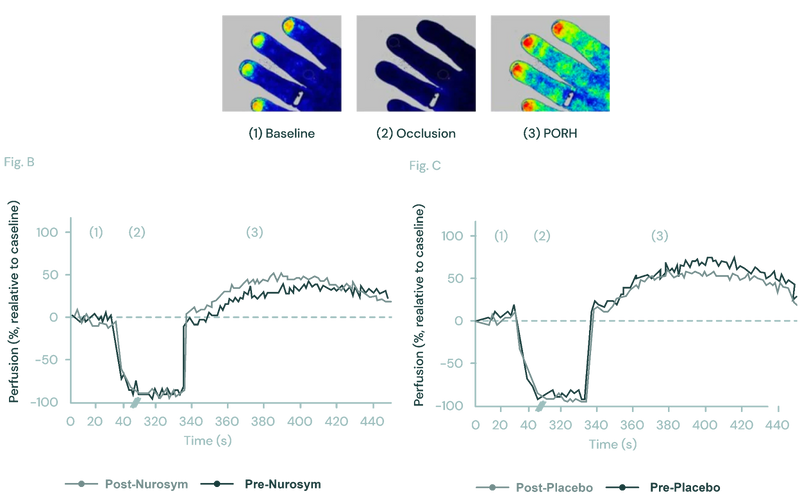
Fig. Effect of the Nurosym neuromodulation on peripheral microcirculation using laser speckle contrast imaging (LSCI). In the LSCI recordings of the left hand dorsum, (1) pseudo colour images showed baseline, (2) occlusion, and (3) post-occlusive reactive hyperemia (PORH) phase. Blue indicated lower, while red indicated higher perfusion rates. Comparing blood perfusion changes over the nail bed area before and after Nurosym neuromodulation (B) and Placebo stimulation (C), significantly higher perfusion rates were observed after Nurosym (Parasym Clinical Trials, doi: 10.1016/j.cardfail.2020.12.017).
In the Nurosym research, patients with atrial fibrillation (AF) experienced an 85% decrease AF burden measure when treated with Nurosym for 6 months, in contrast to Placebo control group (doi: 10.1016/j.jacep.2019.11.008, 10.1161/JAHA.120.020865).
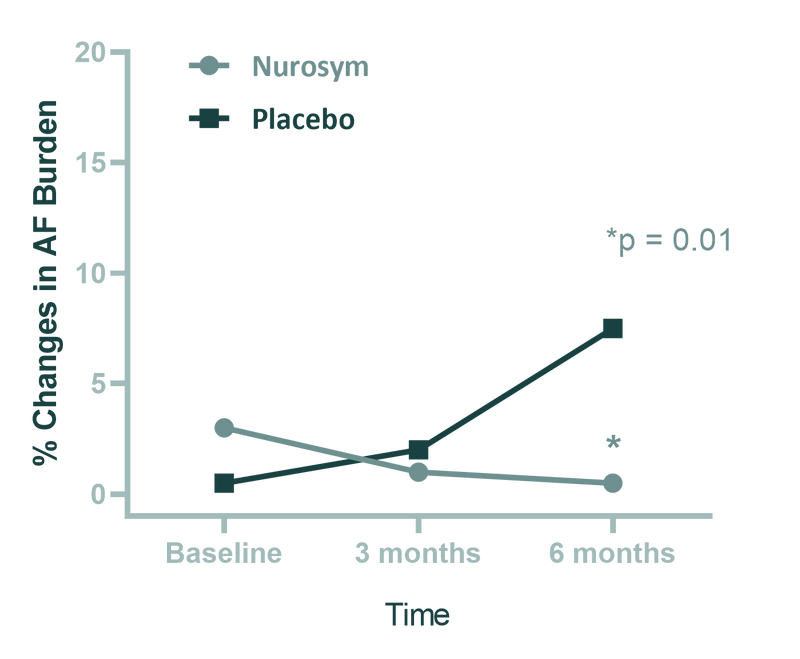
Fig. Comparison of atrial fibrillation (AF) burden between the 2 groups (Nurosym neuromodulation and Placebo stimulation) after 6 months treatment. Patients undergoing Nurosym treatment exhibit higher baseline measurements, indicating a greater improvement. The data are presented as median and interquartile range. The p value is based on a comparison of median AF burden levels at the 6-month time point after adjusting for baseline measures. (Parasym Clinical Trials, TREAT AF).
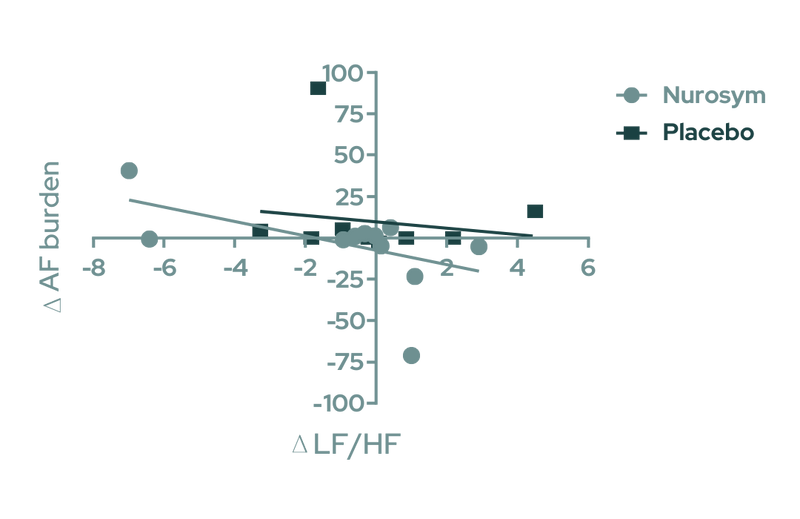
Fig. Association of Heart Rate Variability With the Change in AF Burden. Linear regression of the change in atrial fibrillation (AF) burden at follow-up (Δ AF burden) as a function of the respective change in low frequency to high frequency ratio (Δ LF/HF) in the Nurosym neuromodulation and Placebo control groups.( Parasym Clinical Trials, doi:TREAT AF).
After 3 months of Nurosym treatment, an decrease in deformation of heart muscle (indicated by GLS improvement (left ventricular function) of approximately ~11% was observed compared to the control group, and this improvement was associated with a reduction in cardiovascular disease risk factors (doi: 10.1161/JAHA.121.023582).
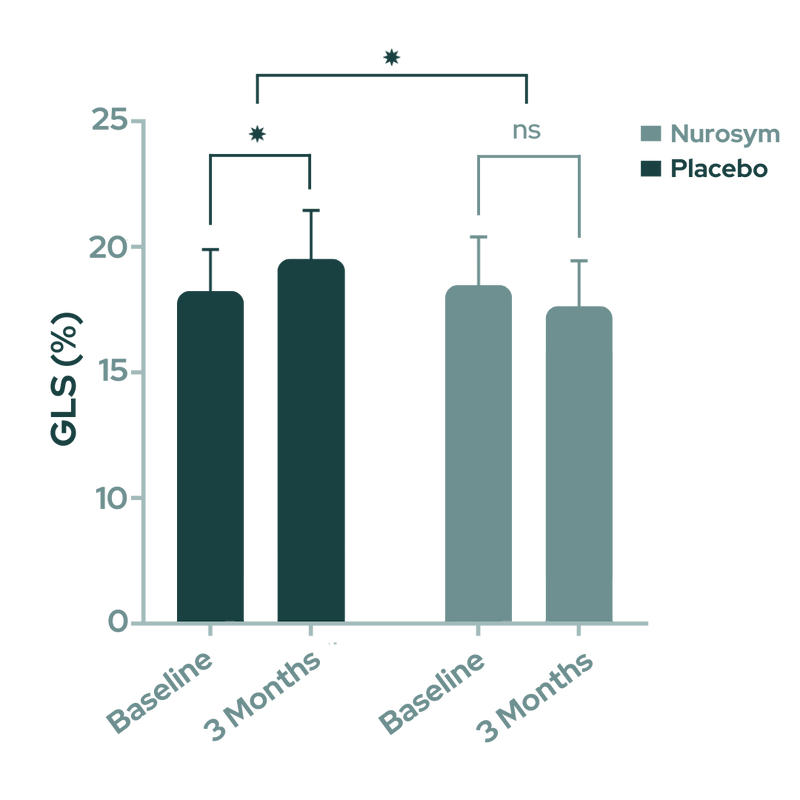
Fig. Changes in global longitudinal strain (GLS). Nurosym neuromodulation indicates significant improvement in GLS parameter, compared to Placebo (*P<0.05) (Parasym Clinical Trials, doi: 10.1161/JAHA.121.023582).
Another research concluded that Nurosym acutely ameliorates cardiac mechanics by modulating the autonomic tone (doi: 10.1007/s12265-018-9853-6).
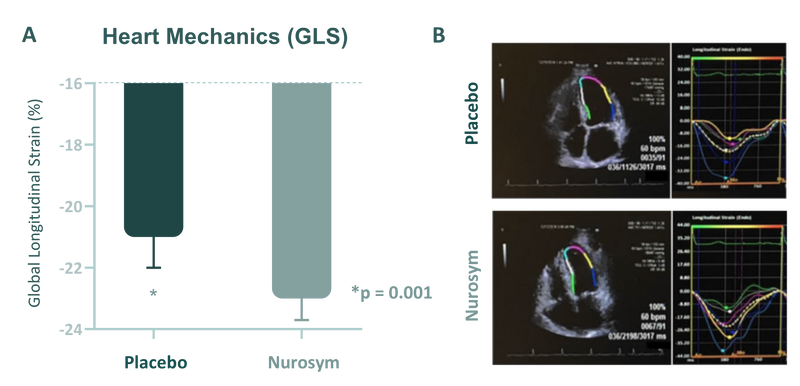
Fig (a, b) When active Nurosym neuromodulation was applied, it led to a reduction in global longitudinal strain, compared to when sham stimulation. A real-life example of strain analysis of the left ventricle (as seen in the apical 4-chamber view) showed that Nurosym neuromodulation (lower panel) had a positive impact compared to sham stimulation (upper panel) on the same patient (doi: 10.1007/s12265-018-9853-6).
Another Nurosym finding highlights 78% reduction in inflammation (cytokines levels like IL-8, Il-6, TNF-α) in patients with Heart Failure With Reduced Ejection Fraction. Decreased inflammation is associated with lower oxidative stress and may contribute to improved cardiac function, reduced myocardial damage (doi: 10.1161/JAHA.121.023582)
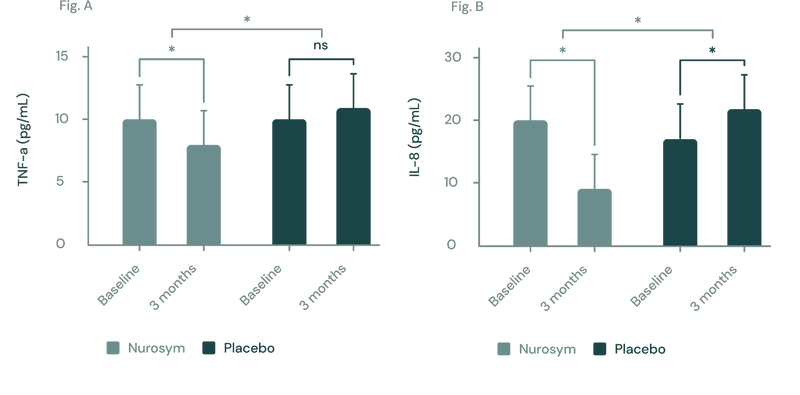
(Figure A, B) In a three-month study employing the Nurosym device for heart failure patients, notable improvements (*P<0.05) were noted in inflammatory biomarkers: (A) Tumor Necrosis Factor (TNF)‐α exhibited a ~23% reduction, while (B) Interleukin (IL)‐8 showed a marked ~61.3% reduction. The investigation specifically targeted participants with elevated baseline inflammation levels (Parasym Clinical Trials, doi: 10.1016/j.cardfail.2022.10.278).
Nurosym neuromodulation helps lower neuropeptide Y (NPY) levels by about 38% in atrial fibrillation progression, compared to Placebo group. Higher NPY is also associated with conditions such as atherosclerosis, heart failure, and arrhythmias, contributing to cardiovascular dysfunction.
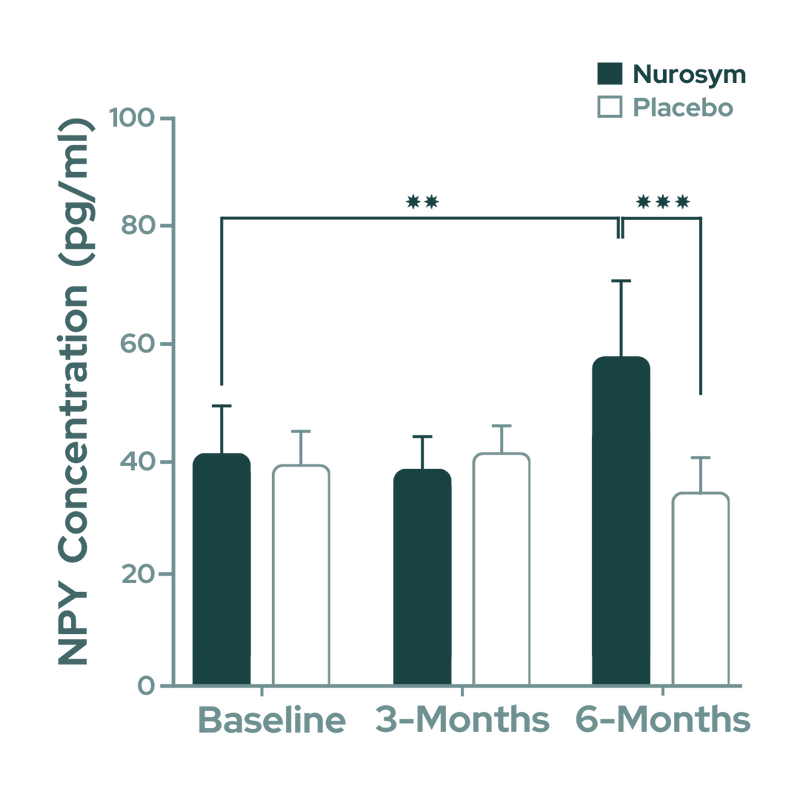
Fig. Significant reduction in circulating neuropeptide Y (NPY) concentrations was observed after 6 months of Nurosym treatment. NPY is associated with atrial fibrillation (AF) progression (Parasym Clinical Trials, doi:j.jacep.2020.08.025).
In the Parasym clinical trial, a 29% reduction in autoantibodies was observed after Neurosym therapy compared to the placebo, and this reduction correlated with improved cardiovascular function and reduced heart damage in postural orthostatic tachycardia syndrome (POTS) (doi: 10.1016/j.hrthm.2023.04.051)
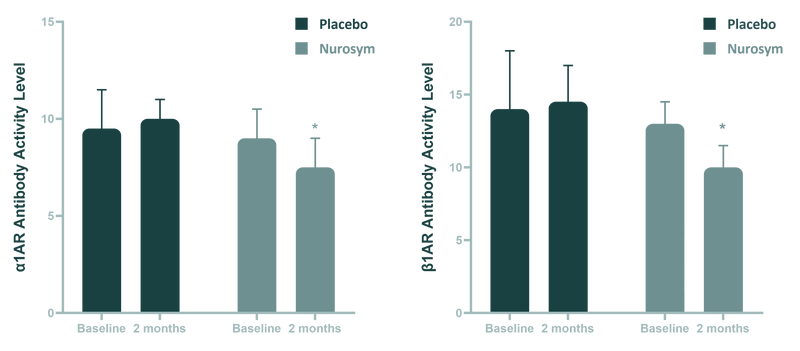
Fig (A, B). Comparison of antiautonomic autoantibody activity between Nurosym neuromodulation and Placebo control at 3 months change. (A) β1-adrenergic (β1AR) autoantibody activity. (B) α1-adrenergic receptor (α1AR) autoantibody activity. P < 0.05. An=antibody. (Parasym Clinical Trials, doi: 10.1016/j.hrthm.2023.04.051).
Nurosym lowered ~24% ROS markers which may minimise oxidative damage to blood vessels and tissues (doi: 10.1007/s10286-023-00997-z).
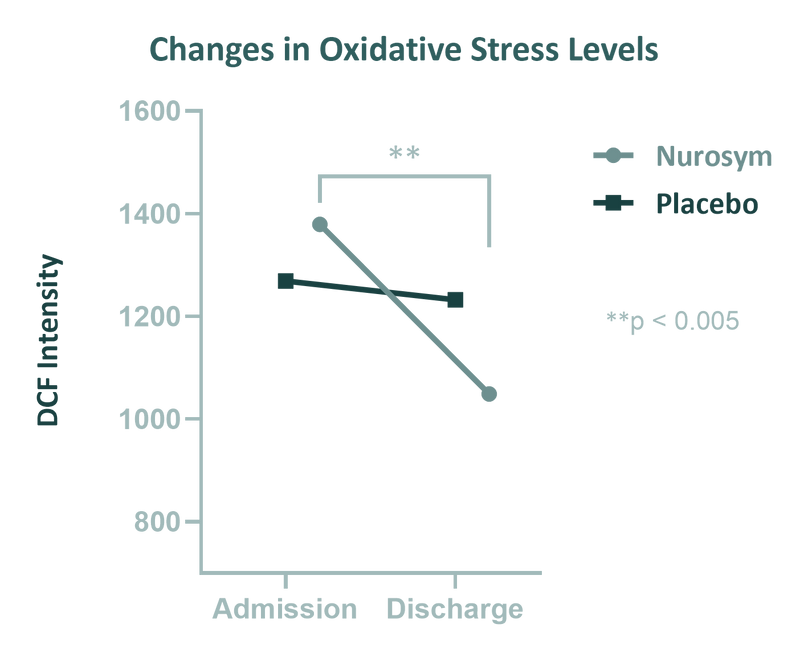
Fig. Effect of LLTS on oxidative stress. A Change in median values of DCF from admission to discharge in Nurosym group compared to control Placebo group (Parasym Clinical Trial, doi: 10.1007/s10286-023-00997-z)
Doctors about Nurosym
Patients about Nurosym
Connie
“Many days I couldn’t even lift my head off the pillow due to my fatigue and Postural tachycardia syndrome (POTS). With the Parasym I now have a tool I can use myself at home which doesn’t have the nasty side effects medications do. My POTS, although still present, is much more manageable. I would recommend it to anyone having vagus nerve issues or symptoms, that is looking for something to help at home”
James
“I am a retired physician, and when I was researching A-Fib I realised that one significant factor was the imbalance of sympathetic & parasympathetic stimulation. I stumbled across articles on the transcutaneous auricular vagus stimulator that was not invasive at all. I was and remain sold on it. Interestingly, It has given me the longest period of being free of A-Fib symptoms I have had”
Who is for it?
Nurosym may alleviate the symptoms associated with cardiovascular conditions such as atrial fibrillation (AF), heart failure, individuals at risk of stroke, and those with hypertension aiming to enhance their endothelial function.
Notably, patients with chronic heart diseases often witness substantial cardiovascular improvements within a 3-month period, including enhanced heart rhythm stability in the case of AF and improved heart rate variability (HRV) after several sessions. It is worth highlighting that individuals with hypertension may also observe enhancements in endothelial function.
Unlike conventional drugs, whose primary aim is symptom management, Nurosym is designed to actively support and optimise cardiovascular system function by activating the parasympathetic nervous system, which exerts antiarrhythmic and blood pressure-lowering effects.
Protocol - How to Use
Research indicates that one hour of Nurosym neuromodulation can improve cardiac mechanics and positively alter sympathovagal balance, making it an effective treatment for heart disease patients. It is recommended to perform a 6-month therapy regimen, as demonstrated in the Parasym study, where Nurosym effectively reduced atrial fibrillation (AF) burden in patients with paroxysmal AF, decreased inflammation and improved endothelial inner lining.
Studies on healthy individuals have shown that even 15 minutes of stimulation can improve autonomic balance, thus preventing cardiovascular diseases. This device is designed specifically to address the neurobiological aspects of heart diseases, offering a non-invasive treatment of vascular and cardiac symptoms through targeted parasympathetic neuromodulation interventions. During Nurosym treatment, it is advisable to monitor potassium levels and maintain them within the normal range, which can further enhance the positive impact of the treatment.
How often
Nurosym is recommended for use twice daily based on clinical research and patient feedback. This regimen ensures optimal energy balancing and nervous system calming.
How long
Users should allocate 30 minutes in the morning and 60 minutes before sleep for Nurosym therapy sessions. Consistency in application is key to achieving desired results.
Results
Positive outcomes from Nurosym therapy may become noticeable within a relatively short timeframe. Many individuals report improvements within days of starting treatment.


