Vagus Nerve and Its Role in Heart Rate Variability (HRV)
The vagus nerve, a fundamental component of the autonomic nervous system, is essential for maintaining the body's physiological health. Without proper activity of the vagus nerve, regulating the body's physiological functions would be impossible. Its reflex pathways regulate the parasympathetic "rest and digest" nervous system, supplying efferent fibres to most organs. The activity of the vagus nerve is closely linked to the high-frequency component of heart rate variability (HRV), serving as a marker of vagal tone. Consequently, any impairment of the vagus nerve can exert repercussions not only on heart performance and cardiac functions but also on the process of recovery and our cognitive functioning. Dysfunction of the vagus nerve can occur due to various factors, including chronic stress, exposure to toxins, intense physical training, injuries, or infections. Here's how vagus nerve dysfunction can leads to:
Dysautonomia
Dysautonomia refers to a dysfunction of the autonomic nervous system. One common manifestation involves impairment of the parasympathetic nervous system, primarily regulated by the vagus nerve. Compromise in the function of the nucleus tractus solitarii (NTS) diminishes the activity of neurons projecting to vagal efferent nuclei, resulting in weakened vagal control and decreased heart rate variability (HRV). This reduction indicates a diminished capacity for effective relaxation and recovery. Dysfunction in heart rate control can disrupt the balance between energy expenditure and recovery, crucial for optimal performance, and may increase fatigue, stress, and anxiety¹.
Impaired Cardiac function
HRV serves as a valuable tool for assessing neurocardiac physiology. A weakened HRV, often resulting from vagus nerve impairment, profoundly affects heart rate modulation. The vagus nerve, which innervates key cardiac structures such as the sinoatrial, atrioventricular nodes, as well as the myocardium, regulates heart rate. When vagal control is insufficient, heart rate regulation becomes compromised. In response, the sympathetic output increases catecholamine secretion, accelerating heart rate and contractility. This imbalance between parasympathetic and sympathetic influences leads to irregularities in heart rhythm, including tachycardia (abnormally fast heart rate) or bradycardia (abnormally slow heart rate). Such rhythm disturbances not only pose immediate health risks but also contribute to long-term cardiovascular complications if left unaddressed².
Reduced Stress Recovery
HRV is widely recognized as a marker of physiological responses to both acute and chronic stressors. Low heart rate variability is indicative of dysregulation in both the affective and autonomic systems, often directly associated with vagal damage. This impairment can significantly impede one's ability to effectively cope with and recover from stress. Consequently, it leads to excessive and chronic activation of the fear or "stress" system, exacerbating cardiac dysregulation and fostering increased anxiety. Conversely, maintaining a high rate of heart rate variability is pivotal in enhancing stress resistance. Failure to adequately modulate the vagus nerve can further worsen the physiological response to stress³.
Increased Inflammation
During inflammation, heart rate variability (HRV) tends to decrease, a phenomenon also observed in individuals with impaired vagal function. The vagus nerve, operating through the cholinergic anti-inflammatory pathway (CAP), plays an indispensable role in regulating inflammation. Damage to the vagus nerve increases the risk of systemic inflammation, compromising the body's ability to effectively manage inflammatory responses. Consequently, individuals with vagal dysfunction may experience heightened fatigue and prolonged recovery times. Thus, the relationship between HRV, vagal function, and inflammation highlights the importance of maintaining optimal vagal tone for promoting immune system functioning⁴.
Reduced Sleep Quality
Very low-frequency HRV was found to be inversely associated with three negative sleep indices: sleep quality, daytime dysfunction, and global sleep assessment. The results showed that damage to the vagus nerve is unfavourably associated with HRV, causing an overactivation disorder of the sympathetic nervous system. This has a direct impact on regeneration in the deep sleep phase and mental health. Additionally, vagal impairment may also affect brain structures involved in sleep regulation, including the nucleus of the solitary tract in the brainstem. This nucleus processes sleep-related sensory information, such as catecholamines and circadian control, which helps maintain energy throughout the day¹.
Increased Pain Perception
HRV is also related to endogenous pain modulation (EPM), a relevant factor in chronic pain development and maintenance. Impairment of the vagus nerve can lead to heightened pain sensitivity due to decreased vagal activity. Decreased vagal activity can disrupt the usual processing of pain signals, resulting in heightened sensitivity to both physical sensations and emotional responses to pain. This heightened perception of pain can present challenges for middle-aged individuals in managing discomfort and may hinder their ability to engage in daily activities comfortably².
Impaired Gastrointestinal Functioning
Based on analyses of HRV, gastrointestinal reflux disease (GERD), and functional gastrointestinal disorders (FGIDs), it was found that they are associated with impaired autonomic dysfunction, mainly due to suppressed vagal and overactive sympathetic tone. The vagus nerve works as a regulator of gastrointestinal function through its parasympathetic innervation of the digestive tract. Impairment of the vagus nerve, as seen in conditions like GERD and FGID, disrupts normal autonomic control over motility and endocrine secretion, resulting in diminished parasympathetic nervous system activation. This can manifest in symptoms such as acid reflux, bloating, abdominal discomfort, and changes in bowel habits⁵'⁶.
- Karemaker J.M. (2022). The multibranched nerve: vagal function beyond heart rate variability. Biological Psychology 172, 108378, 0301-0511.
- Forte G., Troisi G., et al. (2022). Heart Rate Variability and Pain: A Systematic Review. Brain Sci. 12, 153.
- Herman J.P., McKlveen J.M., et al. (2016). Regulation of the Hypothalamic Pituitary Adrenocortical Stress Response. Comprehensive Physiology, 603–621.
- Kvadsheim E., Sørensen L., et al. (2022). Vagally mediated heart rate variability, stress, and perceived social support: a focus on sex differences. Stress, 25(1), 113–121.
- Ali M.K., & Chen J.D.Z. (2023). Roles of Heart Rate Variability in Assessing Autonomic Nervous System in Functional Gastrointestinal Disorders: A Systematic Review. Diagnostics, 13(2), 293.
- Breit S., Kupferberg A., et al. (2018). Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry, 9.
Nurosym stimulates the auricular branch of the vagus nerve through the skin on the ear, contributing to the modulation of autonomic balance. Functional MRI (fMRI) imaging studies have revealed that this stimulation of the vagus nerve activates key brain nuclei, including the nucleus tractus solitarius (NTS) within the vagal nuclei complex along the central vagal projections. Indications of this stimulation include changes in heart rate variability (HRV), a recognized biomarker of vagal tone, which may consequently help manage symptoms associated with dysautonomia. Scientific evidence consistently underscores the association between vagal tone and overall health, relaxation, and emotional states.
Nurosym activates the vagus nerve via its fibres, initiating parasympathetic output and influencing cardiac vagal activity. This influence is reflected in changes in HRV, a well-established biomarker of vagal tone. By exerting inhibitory control over the heart, Nurosym helps maintain heart rate within an optimal range, thereby promoting improved heart rate regulation and reducing sympathetic overactivity. This modulation of autonomic function may contribute to stabilising heart rhythm and preventing episodes of tachycardia or bradycardia.
Nurosym's ability to enhance stress resilience and expedite recovery stems from its capacity to increase heart rate variability (HRV), reflecting improved adaptability to stress and quicker recuperation. By influencing anticipatory HRV, Nurosym demonstrates its efficacy in preparing the body for stressors by regulating prefrontal activity and stress responses beforehand. Nurosym's ability to improve vagus nerve function helps rebalance HPA axis, therefore inflict neurotransmitter levels and enhances cellular stress resilience, resulting in more effective stress management and reduced chronic anxiety. This physiological boost aids in regeneration and mitigates the physical effects of stress, making it valuable for managing stress and promoting optimal recovery, both crucial for longevity.
Research on Nurosym has demonstrated its potential in reducing levels of inflammatory cytokines, such as TNF-α, which is crucial in managing systemic inflammation and enhancing the body's regeneration processes. Given the physiological relation between the vagus and inflammatory processes, one would expect to find higher HRV, especially indices of vagally-mediated HRV, to be associated with decreased levels of inflammation via the cholinergic anti-inflammatory pathway. This is achieved through the activation of the vagus nerve's efferent branch, a key component of the cholinergic anti-inflammatory pathway. HRV can be used to index activity of the neurophysiological pathway responsible for adaptively regulating inflammatory processes in humans.
By modulating the activity of the vagus nerve, Nurosym contributes to the normalisation of sleep patterns. Nurosym's influence varies across sleep stages, promoting higher HRV during REM sleep and mitigating the decrease in HRV typically observed during non-REM sleep. As high-quality sleep is essential for regeneration and energy levels, this modulation of HRV during sleep aids in identifying and addressing sleep disorders or underlying health issues, as well as vagal nerve impairment.
Following Nurosym therapy, patients exhibited a decrease in autonomic response associated with painful stimuli. This effect is likely attributable to Nurosym's capacity to diminish the intensity of nociceptive responses to pain, which correlates with the observed increase in HRV. These findings suggest that modulation of HRV serves as an effective intervention for ameliorating pain sensations and enhancing pain tolerance, potentially offering relief for individuals experiencing chronic pain.
Nurosym restores vagal balance, a pivotal element of the gut-brain axis. This is assessed via HRV, which quantifies enhanced parasympathetic activity and moderated sympathetic tone. Increased HRV correlates with alleviated symptoms such as acid reflux, bloating, abdominal discomfort, and irregular bowel movements resulting from impaired vagal function. This improvement can enhance gastrointestinal motility and endocrine secretion, thereby addressing the underlying autonomic dysregulation in GERD and FGID.
Nurosym Research-Based Evidence
92% of Nurosym patients after 3 months of regular treatment observe positive outcomes in heart rate variability (HRV), which serves as an indicator of an enhanced parasympathetic nervous system response, which contributes to organism recovery and stress resilience.
In the Nurosym research, the neuromodulation group was associated with improved heart rate variability (HRV), including a substantial 61% increase in measures of cardiac vagal activity (HF parameter), along with significant improvements in other parameters (18% RMSSD, 25% pRR50, 14% SDRR), when compared to the placebo group.
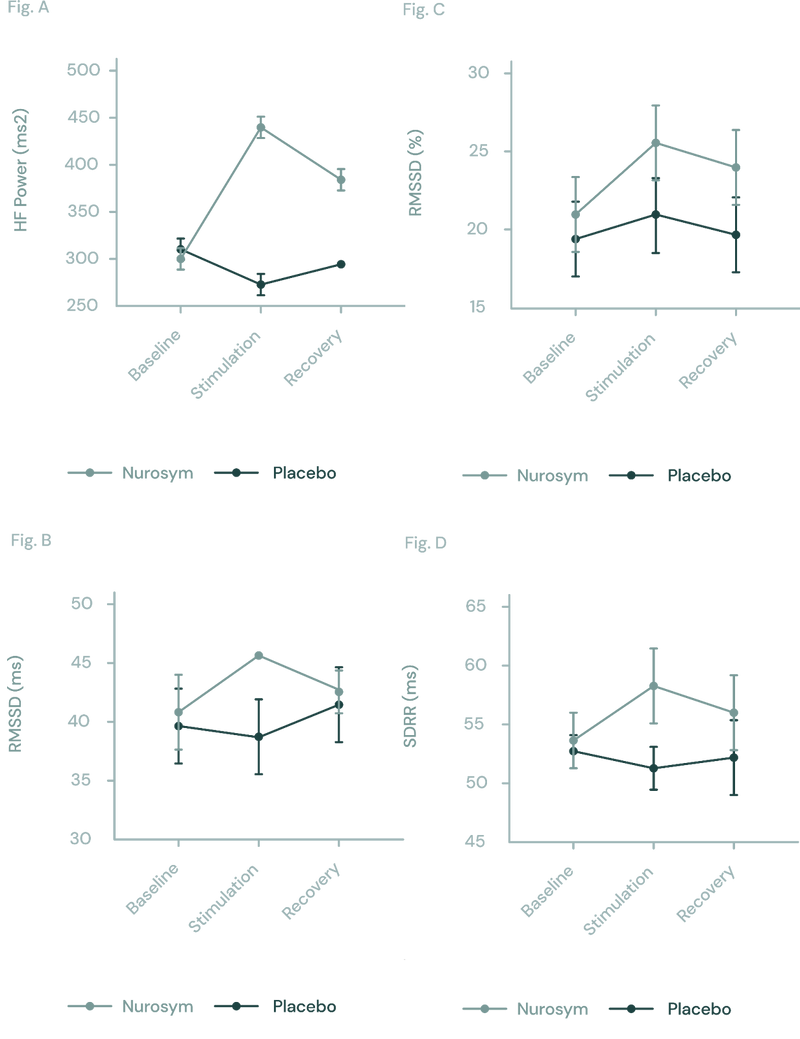
Fig (A, B, C D). The response of autonomic function measured by HRV in Nurosym or Placebo conditions over time: (A) HF, (B) RMSSD, (C) pRR50, (D) SDRR. With Nurosym, the measurements of HF, RMSSD, PRR50 and SDRR were significantly higher than those in Placebo (Parasym Clinical Trials, 2022).
These findings suggest a significant shift towards the parasympathetic side, particularly pronounced in individuals with lower HRV. This heightened relaxation response may enhance both motor and cognitive functionality, especially benefiting individuals who require greater modulation.
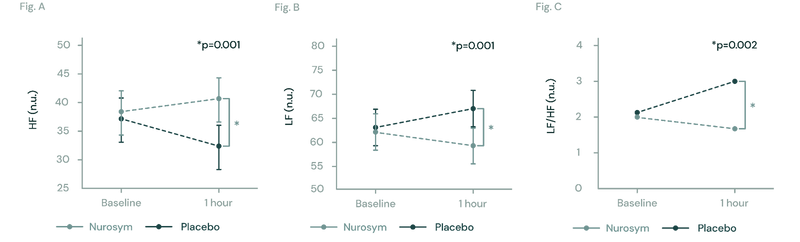
Fig (A, B, C). The figures illustrate changes in heart rate variability (HRV) during Nurosym neuromodulation. In Figure (A), High Frequency HRV significantly increases (*p=0.001). In Figure (B), Low Frequency HRV significantly decreases (*P=0.001). Figure (C) demonstrates that the ratio of LF to HF is significantly decreased (*p=0.002) (Parasym Clinical Trials, 2018).
Atrial fibrillation (AF)commonly occurs in individuals with lower HRV. In the Nurosym study, participants diagnosed with AF experienced a significant 85% reduction in AF burden measures following Nurosym treatment for six months, compared to those in the placebo control group. This reduction in AF burden could be accompanied by an increase in HRV as a potential indicator of improved autonomic balance and cardiac function.
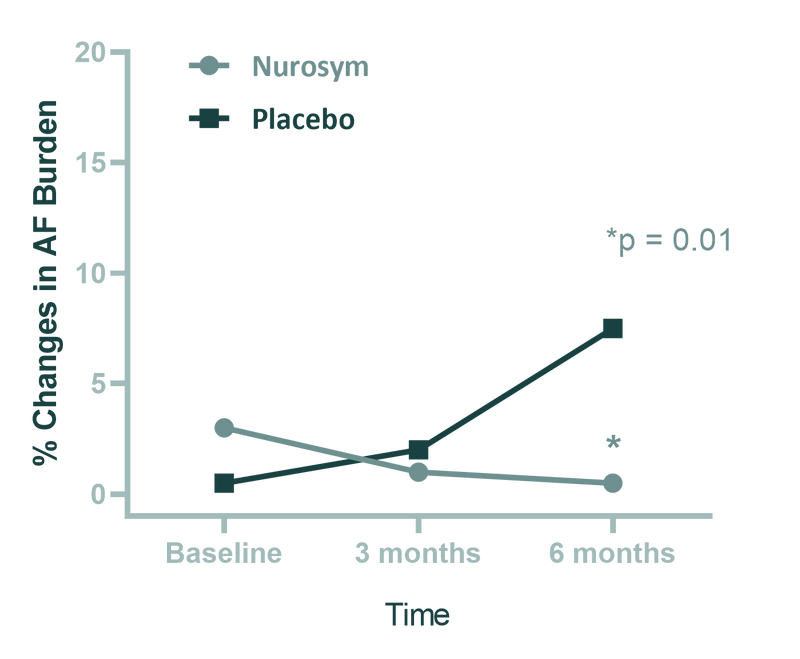
(Fig). Comparison of atrial fibrillation (AF) burden between the 2 groups (Nurosym neuromodulation and Placebo stimulation) after 6 months treatment. Patients undergoing Nurosym treatment exhibit higher baseline measurements, indicating a greater improvement. The data are presented as median and interquartile range. The p value is based on a comparison of median AF burden levels at the 6-month time point after adjusting for baseline measures. (Parasym Clinical Trials, 2020).
After 3 months of Nurosym treatment, a decrease in the deformation of the heart muscle (higher GLS) of ~19% was observed compared to the control group. This improvement may be attributed to increased HRV and is associated with a reduction in cardiovascular disease risk factors.
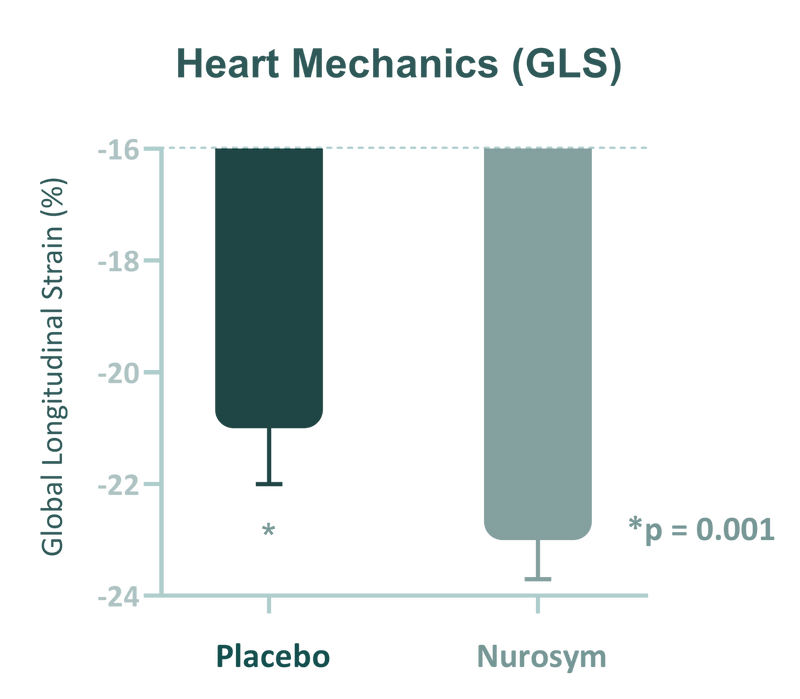
Fig. Changes in global longitudinal strain (GLS). Nurosym neuromodulation indicates significant improvement in GLS parameter, compared to Placebo (*P<0.05) (Parasym Clinical Trials, ).
The pro-inflammatory state has been associated with a decrease in total power HRV, including vagally-mediated HRV indices. Research on Nurosym suggests a reduction of up to 78% in inflammation, as evidenced by decreased levels of cytokines such as IL-8, IL-6, and TNF-α. This reduction in inflammation may be correlated with higher HRV levels, indicating increased activity in the cholinergic anti-inflammatory pathway.
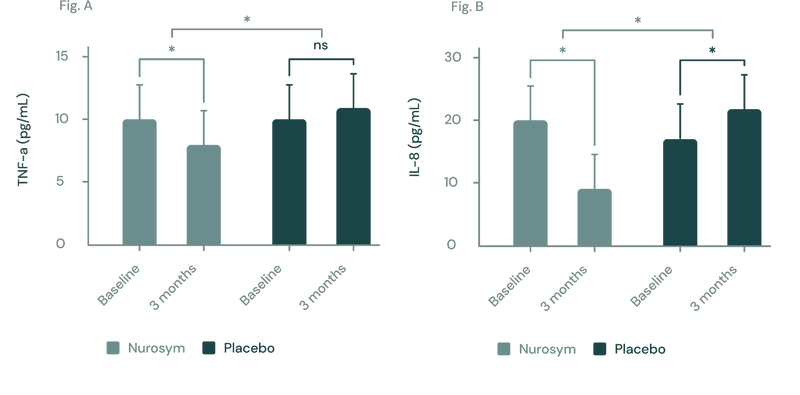
(Figure A, B) In a three-month study employing the Nurosym device for heart failure patients, notable improvements (*P<0.05) were noted in inflammatory biomarkers: (A) Tumor Necrosis Factor (TNF)‐α exhibited a ~23% reduction, while (B) Interleukin (IL)‐8 showed a marked ~61.3% reduction. The investigation specifically targeted participants with elevated baseline inflammation levels (Parasym Clinical Trials, 2022).
Doctors about Nurosym
Patients about Nurosym
Natalie
“Parasym was recommended to me by my cranio osteopath. I have been dealing with chronic fatigue syndrome/burn-out and chronic insomnia for over 25 years. I am also a HeartMath Institute Certified coach for HRV coherence resilience training. It was my first career in the financial markets on the trading floor that ignited the over-activated stress response 30 years ago. It has been a long journey of discovery in restoring my health with different modalities. I started using Parasym in July 2021 with positive results and with science-based evidence of its impact. My sleep has improved significantly but there is still much work being done holistically to restore homeostasis. One of the most profound experiences to report is that I have been using Parasym together with HeartMath Institute's Inner Balance biofeedback app and have seen a remarkable impact on my ability to achieve HRV coherence more easily and consistently. This independent biofeedback tool showing the physiological benefits of Parasym in stimulating the vagus nerve and subsequent impact on HRV coherence has encouraged me to use Parasym on a regular basis at least morning and night.”
Who is for it?
Nurosym offers a non-invasive means of rebalancing the autonomic nervous system, potentially yielding significant health benefits for those navigating stress-related health challenges or seeking preventive measures against age-related autonomic dysfunction. This imbalance, often can be seen by stressful lifestyles, can hinder one's ability to adapt to challenges effectively. It's important to recognize that the sympathetic nervous system becomes increasingly reactive with age, underscoring the preventive value of utilising Nurosym to influence heart rate variability (HRV). Given that HRV is closely linked to various health conditions including stress, cardiovascular disease, diabetes, and inflammation, enhancing HRV through Nurosym neuromodulation may offer significant health benefits for individuals contending with these issues.
Protocol - How to Use
Based on the research results, Nurosym neuromodulation sessions should be planned according to the body's needs, adapted to the specific effect we want to achieve. The vagus nerve is most sensitive to modulation in the morning, which coincides with the period of lowest heart rate variability (HRV). Therefore, morning sessions are recommended for most patients. It is worth noting that in the evening the body naturally shows increased HRV. Therefore, for healthy individuals seeking preventive benefits, morning sessions are likely to be most effective and may be sufficient. Evening sessions are recommended for patients who have difficulty relaxing and falling asleep, as well as for people with comorbidities. To optimise therapeutic effects, short stimulation sessions, preferably lasting 15 minutes, repeated four times a day are recommended. Studies have shown that the vagus nerve is activated just 5 minutes after stimulation. Therefore, shorter but more frequent Nurosym sessions may be of greater benefit to patients seeking to increase HRV.
How often
Nurosym is recommended for use twice daily based on clinical research and patient feedback. This regimen ensures optimal energy balancing and nervous system calming.
How long
Users should allocate 30 minutes in the morning and 60 minutes before sleep for Nurosym therapy sessions. Consistency in application is key to achieving desired results.
Results
Positive outcomes from Nurosym therapy may become noticeable within a relatively short timeframe. Many individuals report improvements within days of starting treatment.


