Vagus Nerve and Its Role in Autoimmune Conditions
Autoimmune diseases arise when the body's immune system mistakenly attacks its own tissues, leading to a range of chronic symptoms. These conditions commonly involve chronic inflammation, digestive issues, heart rhythm disturbances, pain, difficulty concentrating, and persistent fatigue, all of which can be influenced by the vagus nerve. This nerve is a key component of the parasympathetic response, including the cholinergic anti-inflammatory pathway, the brain-gut axis, and the hypothalamic-pituitary-adrenal axis. The role of the vagus nerve in various immune-mediated inflammatory diseases, including rheumatoid arthritis, diabetes, primary Sjögren's syndrome, inflammatory bowel disease, and adrenal insufficiency, has been extensively studied, revealing a trend of decreased vagal tone in these conditions. Inflammation of the vagus nerve, which may result from allergies, infections, or toxins, can significantly influence the development and progression of autoimmune diseases, often correlating with chronic inflammation and dysautonomia by¹:
Reduced Heart Rate Variability (HRV)
The most common complication of rheumatoid arthritis (RA) and the one associated with high mortality are disorders of the autonomic cardiovascular system. Heart rate variability (HRV) is a measurement of the central autonomic drive (activity) of the heart muscle. In vagus nerve lesions, a decrease in HRV was observed, which indicates an abnormal and insufficient adaptability of the autonomic nervous system and is associated with a high risk of cardiovascular events².
Inflammatory Response
The vagus nerve plays a critical role in the inflammatory reflex, regulating immune function, and inhibiting excessive production of proinflammatory cytokines and autoantibodies. When the vagus nerve is damaged, this balance often shifts towards chronic inflammation, leading to tissue damage and cell death. Such imbalances are seen in diseases such as inflammatory bowel disease (IBD) and rheumatoid arthritis. High levels of pro-inflammatory cytokines and autoantibodies are often associated with increased activity and severity of autoimmune disease symptoms, as well as commonly seen comorbidities such as cardiovascular issues (e.g., ischemic heart disease, heart failure, arrhythmias)¹.
Neurogenic Inflammation
Impaired function of the vagus nerve can significantly contribute to neurogenic inflammation, a form of inflammation primarily mediated by the nervous system, which can lead to pathology in allergies and autoimmune disease. Inadequate regulation of inflammation during dysfunction of the vagus nerve can contribute to the progression and severity of autoimmune diseases. This can also increase pain perception and tissue sensitivity, particularly in conditions like Inflammatory Bowel Disease (IBD) and Rheumatoid Arthritis (RA)³.
Impaired Gastrointestinal Functioning
The vagus nerve, as an integral part of the neuroendocrine-immune axis, is controlling gastrointestinal motility, pancreatic endocrine and exocrine secretion, hepatic glucose production, and other visceral functions. Disruption in vagus nerve function can amplify inflammatory signals from the gut, possibly heightening the vulnerability to autoimmune reactions. In the context of IBD and diabetes, this includes altered intestinal motility and disrupted endocrine and exocrine secretion, exacerbating gastrointestinal problems. These symptoms often extend beyond the gut and manifest as fatigue, increased stress, depression, and cardiovascular abnormalities⁴.
Increased Pain Perception
Damage to the vagus nerve reduces the nerve's ability to not only exacerbate inflammation, but also increases pain sensitivity due to increased neuronal sensitization and inflammation, which may accelerate the progression of immune diseases. The lack of inhibition of pain pathways by the vagus nerve further increases the perception of pain, contributing to the development of chronic pain typically seen in autoimmune diseases. Patients with Rheumatoid Arthritis (RA) and systemic sclerosis (SSc) often experience physical disability due to persistent inflammation. which ultimately leads to deformities and chronic pain. Chronic pain significantly affects the quality of life of patients with autoimmune disease and may contribute to mental illnesses⁵.
- Pavlov V., & Tracey K. (2012). The vagus nerve and the inflammatory reflex—linking immunity and metabolism. Nat Rev Endocrinol 8, 743–754.
- Breit S., Kupferberg A., et al. (2018). Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry, 9.
- Chiu I., von Hehn C. & Woolf C. (2012). Neurogenic inflammation and the peripheral nervous system in host defense and immunopathology. Nat Neurosci 15, 1063–1067.
- Han Y., Wang B., et al. (2022). Vagus Nerve and Underlying Impact on the Gut Microbiota-Brain Axis in Behavior and Neurodegenerative Diseases. J Inflamm Res. 15, 6213-6230.
- Bellocchi C., Carandina A., et al. (2022). The Interplay between Autonomic Nervous System and Inflammation across Systemic Autoimmune Diseases. Int. J. Mol. Sci. 23, 2449.
Nurosym improves the regulatory functions of the vagus nerve, effectively mitigating complications in Rheumatoid Arthritis (RA), as indicated by the improved Heart Rate Variability (HRV). The observable increase in HRV during Nurosym stimulation indicates a more pronounced parasympathetic "rest and digest" activity, signifying good cardiac adaptability. Nurosym's role in enhancing HRV addresses these issues by reestablishing autonomic control processes, leading to a reduced risk of developing cardiovascular complications, such as ischemic heart disease, heart failure, and arrhythmia in individuals with autoimmune conditions.
Autoantibodies are antibodies produced by the immune system that target and attack the body's own cells and tissue.Nurosym demonstrated a reduction in the levels of anti-autonomic autoantibodies (a1-AR and b1-AR), which can be beneficial according to rheumatoid arthritis (RA), Sjögren's syndrome, and lupus. These autoantibodies adversely affect the nervous system by targeting adrenergic receptors. Additionally, research on Nurosym has shown its potential to reduce levels of inflammatory cytokines (IL-6, TNF-α), which may be crucial in treating the systemic inflammation commonly seen in autoimmune diseases. Vagal efferent fibres, when activated, reduce cytokine production via nicotinic receptors on macrophages through the cholinergic anti-inflammatory pathway. Nurosym by activating the vagus nerve inhibits immune cells and signalling molecules. By reducing systemic inflammation, Nurosym may not only alleviate the occurrence and progression of autoimmune diseases but also reduce the perception of pain, thereby improving the daily functioning of affected individuals.
Mitigating Neurogenic Inflammation
Nurosym research has indicated that reduced inflammation involves neuropeptides like Neuropeptide Y (NPY), leading to a decrease in inflammatory responses. Clinical studies have suggested a role for NPY in other immune disorders, such as asthma and arthritis. Nurosym could help in reducing neurogenic inflammation by impacting the function of the vagus nerve and the pathways involving neuropeptides. This stimulation promotes the restoration of synergy between the sympathetic and parasympathetic branches of the autonomic nervous system (ANS). This could lessen tissue sensitivity, swelling, itching, and pain perception, which are significant issues in conditions like Rheumatoid Arthritis (RA), Systemic Sclerosis (SSc), Lupus, and Psoriasis.
Nurosym normalises the functioning of the gastrointestinal tract and pancreas by activating the vagus nerve, thereby improving its tone. The vagus nerve, a crucial part of the central nervous system (CNS), connects to the brain-gut axis, providing parasympathetic innervation to the gastrointestinal tract and pancreas. Nurosym has been shown to positively affect gastrointestinal functions, such as enhancing motility and enzyme secretion. This can potentially alleviate gastrointestinal symptoms and reduce systemic effects like fatigue and stress. Additionally, acting on the central vagal circuitry may also lessen nausea and vomiting, as well as inflammation, which could lead to improvements in conditions such as inflammatory bowel disease (IBD) and type 2 Diabetes.
Nurosym may help treat pain in autoimmune diseases by enhancing the role of the vagus nerve in pain suppression or by reducing neuronal sensitization and inflammation. Stimulation of the auricular branch of the vagus nerve can modulate the activity of the nucleus of the solitary tract, which has major afferent projections to the locus coeruleus that regulate pain threshold. The analgesic effect may also result from a direct effect on autonomic regulatory pathways in the brainstem. This may be particularly valuable in the treatment of chronic pain, thereby improving the quality of life and sleep in patients with RA and SSc.
Nurosym Research-Based Evidence
76% of Nurosym patients after 3 months of regular treatment observe positive outcomes in autoimmune disease, associated with a reduction in sympathetic over-activity, alleviation of pain, mitigation of chronic inflammatory response and oxidative stress, as well as an improvement in mental health characterised by reduced symptoms of depression, fatigue and insomnia.
Low HRV is associated with impaired immune system functioning. In the Nurosym study, the participants who underwent neuromodulation demonstrated significant improvements in heart rate variability (HRV), with a substantial 61% increase in measures of cardiac vagal activity (HF parameter), along with significant improvements in other parameters (18% RMSSD, 25% pRR50, 14% SDRR), when compared to the placebo group.
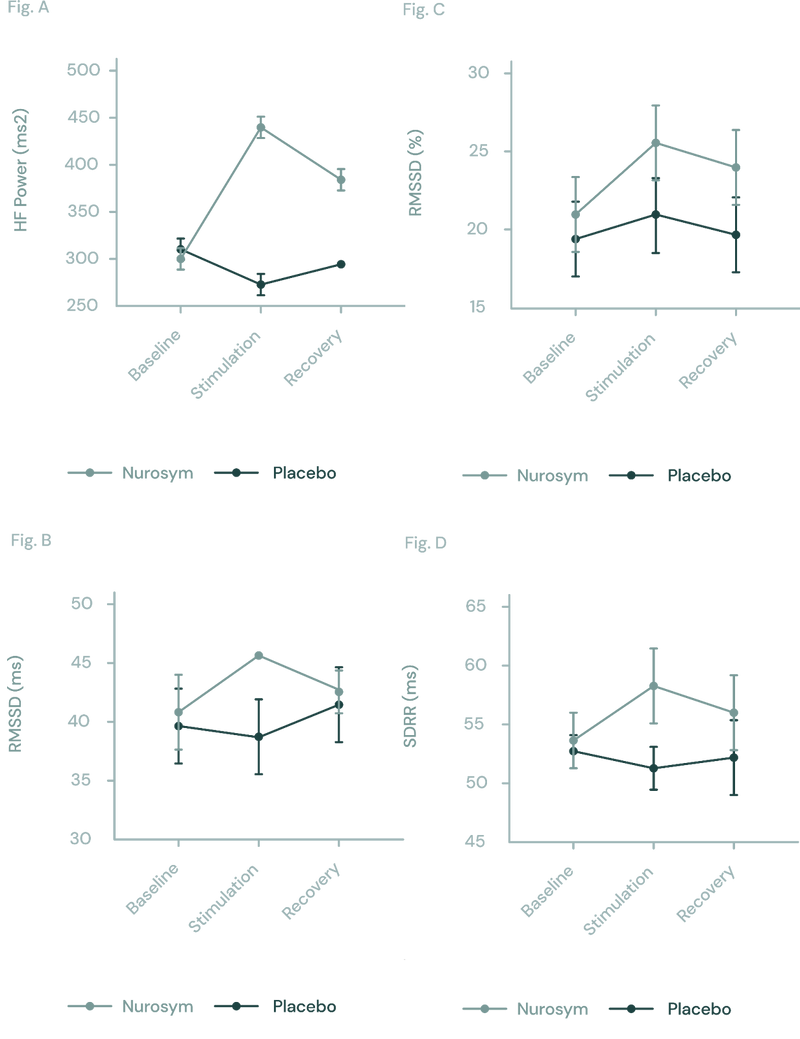
Fig (A, B, C D). The response of autonomic function measured by HRV in Nurosym or Placebo conditions over time: (A) HF, (B) RMSSD, (C) pRR50, (D) SDRR. With Nurosym, the measurements of HF, RMSSD, PRR50 and SDRR were significantly higher than those in Placebo (Parasym Clinical Trials, 2022).
In a Nurosym study, the active arm exhibited reduced levels of anti-autonomic autoantibodies (α-1AR and (β-1AR) by 29% compared to the sham arm at 2 months. This reduction can serve as an indicator of a decrease in the immune system's tendency to form immune complexes – clusters of antibodies bound to antigens.
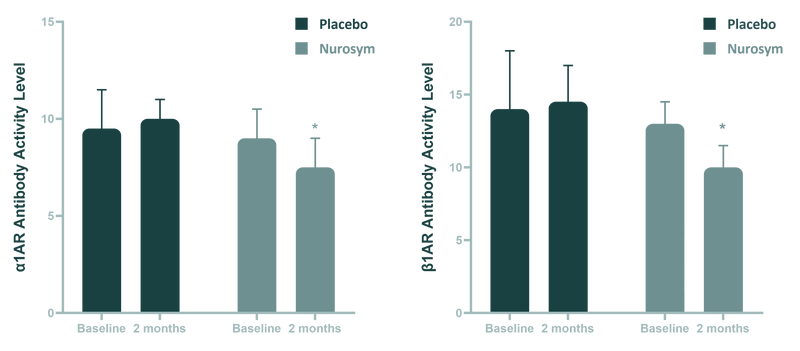
Fig (A, B). Comparison of antiautonomic autoantibody activity between Nurosym neuromodulation and Placebo control at 3 months change. (A) β1-adrenergic (β-1AR) autoantibody activity. (B) α1-adrenergic receptor (α-1AR) autoantibody activity. P < 0.05. An=antibody. (Parasym Clinical Trials, 2023).
Another Nurosym finding highlights 78% reduction in inflammation in IL-6 (and other cytokines levels like ~61% IL-8, ~23% TNF-α). Decreased inflammation can lower fatigue, joint pain, skin rashes and fever.
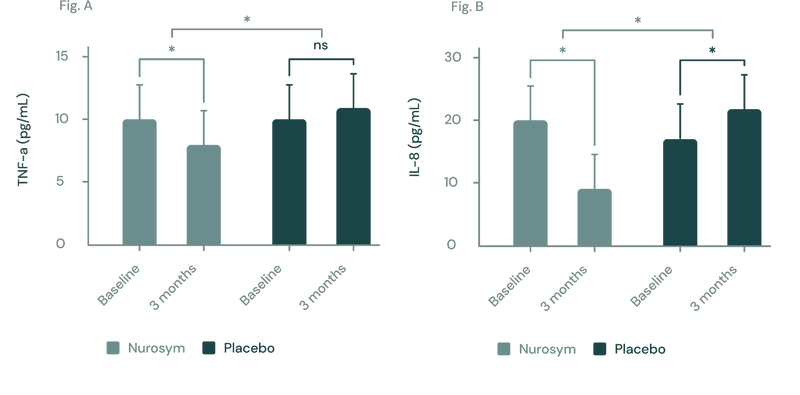
(Figure A, B) In a three-month study employing the Nurosym device for heart failure patients, notable improvements (*P<0.05) were noted in inflammatory biomarkers: (A) Tumor Necrosis Factor (TNF)‐α exhibited a ~23% reduction, while (B) Interleukin (IL)‐8 showed a marked ~61.3% reduction. The investigation specifically targeted participants with elevated baseline inflammation levels (Parasym Clinical Trials, 2022).
Nurosym neuromodulation helps lower neuropeptide Y (NPY) levels by about 38% compared to Placebo group, which may influence the neuroimmune axis in autoimmune conditions.
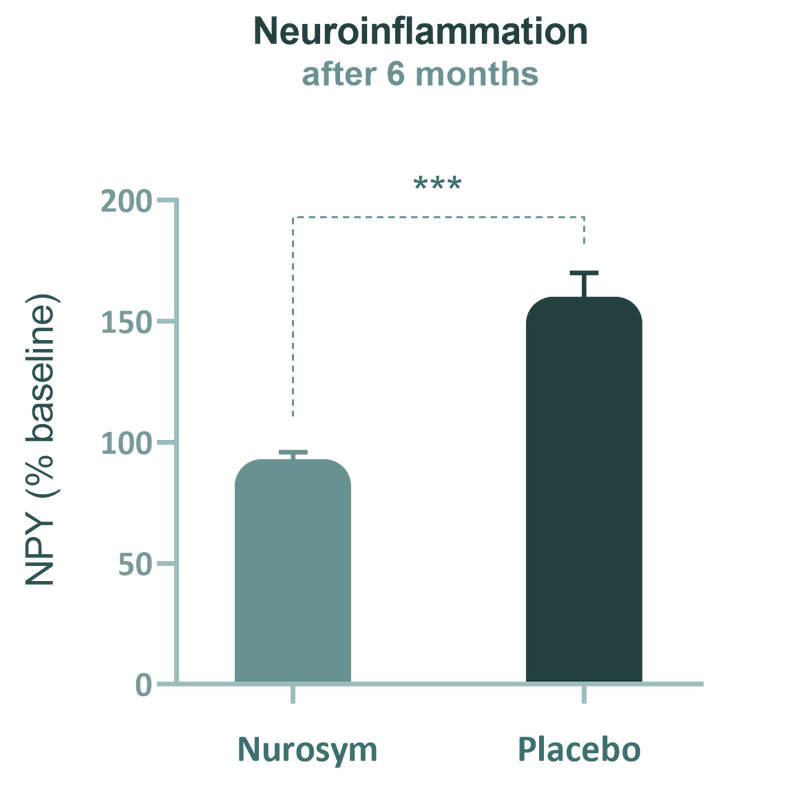
(Fig). Significant reduction in circulating neuropeptide Y (NPY) concentrations was observed after 6 months of Nurosym treatment. NPY is associated with inflammatory disease progression (Parasym Clinical Trials, 2020).
During Parasym trials, reduction of 45% on the Beck Depression score was observed on dysautonomia patients.
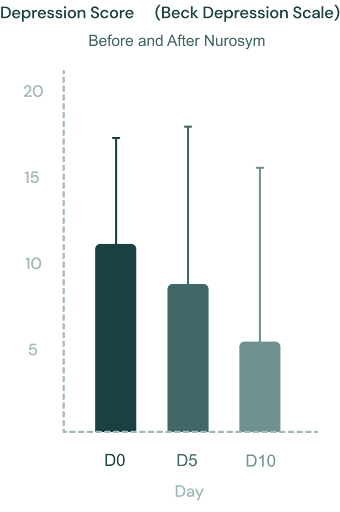
Fig. Evolution of the Beck depression scale scores during Nurosym treatment (day 0, day 5 and day 10). The individual values and the median are shown. Non parametric Friedman statistics for paired comparisons were used and followed by post-hoc Dunn’s multiple comparisons test (Parasym Clinical Trial, 2021).
The Parasym research findings revealed a 48% improvement in fatigue, suggesting positive energy outcomes for autoimmune patients.
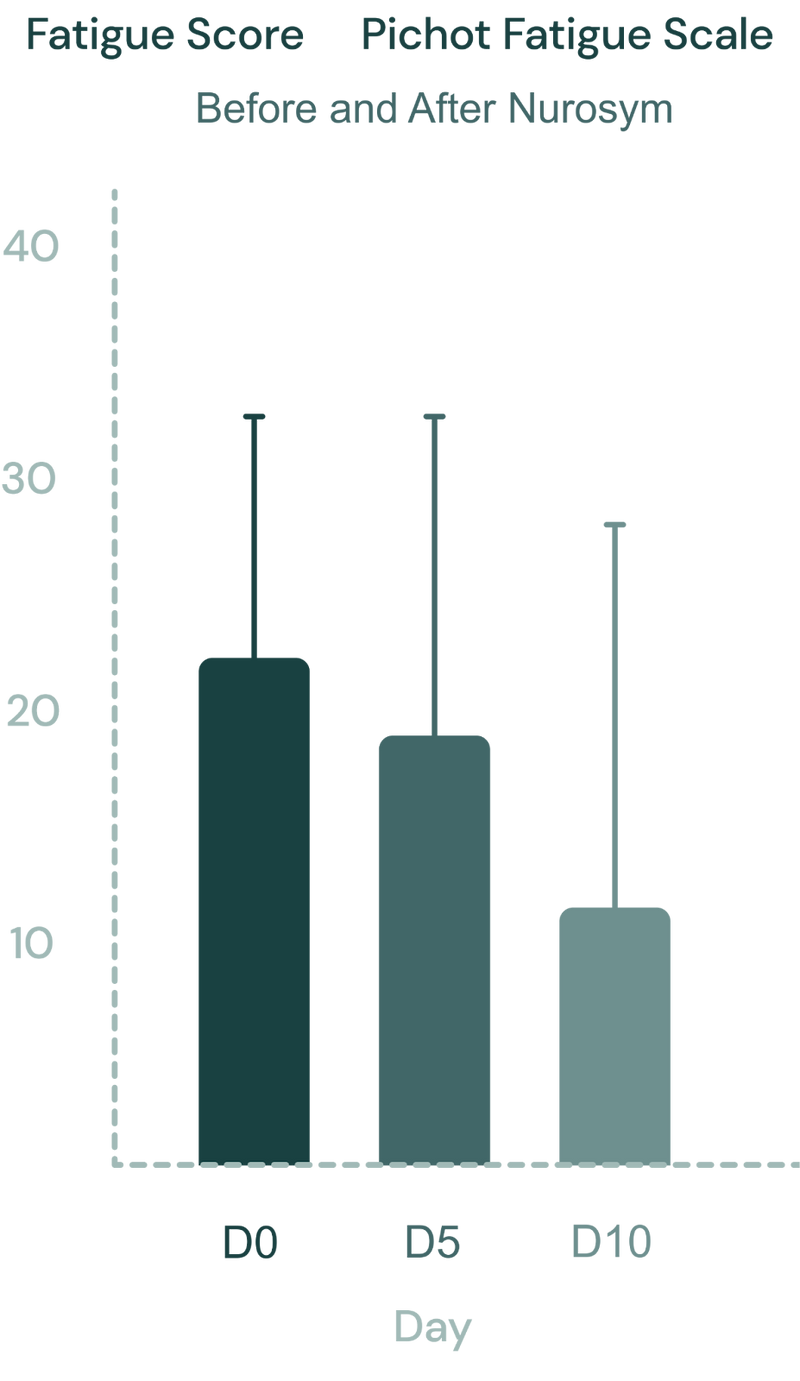
Fig. The Pichot fatigue scale scores during Nurosym therapy (D0: day 0, D5: day 5 and D10: day 10). Significant improvement in fatigue scores after Nurosym treatment was observed (D0 vs. D10, p<0.0001). (Parasym clinical trial, 2021).
Doctors about Nurosym
Patients about Nurosym
“(...) That post viral fatigue went on to develop into an autoimmune disease. So I ordered the [Nurosym; formerly Parasym] device and I've been using that ever since. I tend to use it mostly once a day, sometimes twice a day if I've got the time, but I particularly use it at night time and I use it as part of my bedtime routine. I definitely noticed when I haven't used it, I don't sleep as well. And I have noticed that overall I feel like it lowers the inflammation in my body because when I don't use it, I feel a lot more inflamed and achy and just just not well. So yeah, I'm really, really happy with the device."
Tatiana
“Nurosym helped soothe the multiple inflammatory conditions I had developed after covid, such as arthritis, myocarditis, thyroiditis and brain fog. As I now feel better, I do not need to use it every day anymore, but I still incorporate it in my routine whenever I feel the need to relax and restore my nervous system and my whole body.”
“I'm a long COVID sufferer…I had a lot of muscle spasms, and I was also overly sensitive to external stimuli. So some days I couldn't do anything but just lay down with noise cancelling headphones and dim the light. And that changed after I started using [Nurosym; formerly Parasym] on a daily basis… So, for me, it has been an excellent treatment and I'm thankful for that.”
Who is for it?
Nurosym proves beneficial for individuals dealing with autoimmune conditions, marked by persistent symptoms like fatigue, cognitive impairment, and autonomic dysfunction. It works to rebalance the autonomic nervous system, reduce inflammation, and relieve neurological symptoms. This makes it a suitable therapeutic option for those facing the enduring consequences of autoimmune disorders. Nurosym successfully improves cognitive and physiological functions in individuals with autoimmune conditions, especially in cases where conventional pharmacological methods fall short, offering only temporary relief for symptoms without contributing to the enhancement of the body's autonomic efficiency.
Protocol - How to Use
Based on research results and patient experiences, it is recommended to administer Nurosym sessions for the treatment of autoimmune diseases, lasting at least 30 minutes twice daily. The vagus nerve is stimulated when a slight tingling sensation is felt at the tragus. Adjusting the duration and frequency of Nurosym sessions is based on individual responses.
Nurosym allows for long-term optimization of quality of life, emphasising the fight against inflammation until remission is achieved. In autoimmune diseases, notable results in reduced inflammation are often observed after 3 months, with quicker relief from pain and depression symptoms. Some patients may begin to notice improvement within 5 days, especially in symptoms of fatigue and pain. Continuing therapy beyond this initial period is beneficial due to its antioxidant properties, with further positive health implications.
How often
Nurosym is recommended for use twice daily based on clinical research and patient feedback. This regimen ensures optimal energy balancing and nervous system calming.
How long
Users should allocate 30 minutes in the morning and 60 minutes before sleep for Nurosym therapy sessions. Consistency in application is key to achieving desired results.
Results
Positive outcomes from Nurosym therapy may become noticeable within a relatively short timeframe. Many individuals report improvements within days of starting treatment.


