Insomnia and the Vagus Nerve Connection
Insomnia, the prevalent sleep disorder, is often linked to disruptions in the autonomic nervous system, where the vagus nerve plays a crucial role. Disturbed sleep patterns can lead to fatigue, daytime sleepiness, emotional instability, and an increased risk of chronic diseases. Symptoms of an overactive nervous system leading to insomnia may include difficulty falling asleep, persistent thoughts before sleep, anxiety, frequent awakenings and restless sleep. These issues may be associated with vagus nerve impairment due to:
Altered “Rest and Digest” Parasympathetic Activation
Vagus nerve plays a crucial role in regulating the body's response to sleep patterns. When impaired, it can lead to a diminished "rest and digest" state measured by reduced vagal tone. This results in an overactive sympathetic nervous system, contributing to difficulties in falling and staying asleep, and prolonged stress responses. Consequently, disruptions in sleep control centres may occur, potentially contributing to difficulties in achieving slow-wave sleep, responsible for physical, immune and memory restorative processes¹.
Disrupted Heart Rate Variability (HRV)
Vagus nerve impairment may impede the enhancement of vagal tone, affecting HRV and correlating with decreased sleep quality. The compromised signals from the vagus nerve could disrupt the modulation of internal circadian rhythms, crucial for maintaining proper sleep-wake cycles, and contribute to nighttime breathing disorders, potentially leading to conditions such as sleep apnea²'³.
Dysregulation of Stress Response
Insomnia often arises from the overactivity of the HPA axis, presenting a significant risk factor for vagus nerve dysfunction. Impaired function of the vagus nerve may contribute to prolonged activation of the stress response system and elevated levels of stress hormones over an extended period. This could potentially reduce the efficacy of stress resilience mechanisms, leading to an increased vulnerability to stress-induced insomnia and disruption in sleep patterns⁴.
Impact on Inflammatory Response
Symptoms of stress and depression can be induced by disruptions in the vagus nerve's regulatory role in the inflammatory response. The inflammatory overactivity, particularly in the gastrointestinal tract, may hinder the absorption of tryptophan, a crucial precursor for neurotransmitters like serotonin that play a pivotal role in governing sleep and digestion. Depletion of these neurotransmitters due to inflammation can further contribute to insomnia, hinder vagal function, and worsen the impact on mental health⁵.
Downregulation of Specific Brain Structures
Vagus nerve impairment may impact on brain structures involved in sleep regulation. This impairment may impact the solitary tract nucleus in the brainstem, which processes sensory information related to sleep like catecholamines, circadian control, sleep apnea, potentially affecting synaptic plasticity, autonomic balance, and overall sleep patterns⁶. The confirmed role of the vagus nerve in sleep regulation, through its influence on neurotransmitter concentration, has been used in treating insomnia⁷.
- Porges S. W. (1995). Cardiac vagal tone: A physiological index of stress. Neuroscience & Biobehavioral Reviews, 19(2), 225–233.
- Tsai H.J., Kuo T.B.J., et al. (2021). Difficulty in initiating sleep is associated with poor morning cardiovascular function. Psychiatry Res. 529, 113518.
- Verrier R. L., & Josephson M. E. (2009). Impact of Sleep on Arrhythmogenesis. Circulation: Arrhythmia and Electrophysiology, 2(4), 450–459.
- Breit S., Kupferberg A., et al. (2018). Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry, 9.
- Pavlov V. & Tracey K. (2012) The vagus nerve and the inflammatory reflex—linking immunity and metabolism. Nat Rev Endocrinol 8, 743–754.
- Bisogni V., Pengo M.F., et al. (2016). The sympathetic nervous system and catecholamines metabolism in obstructive sleep apnoea. J Thorac Dis 8(2), 243-254.
- Wu Y., Song L., et al. (2022). Transcutaneous Vagus Nerve Stimulation Could Improve the Effective Rate on the Quality of Sleep in the Treatment of Primary Insomnia: A Randomized Control Trial. Brain Sci. 12, 1296.
Regular Nurosym sessions balance the sympathetic and parasympathetic nervous systems by stimulating the vagus nerve. When signals stimulate the parasympathetic system, it activates the solitary tract nucleus in the brainstem, which processes sensory information. This nucleus then sends signals to structures related to sleep, called sleep control centres, and brain regions involved in arousal and awareness, potentially contributing to the generation of slow-wave sleep.
Nurosym enhances the activity of the vagus nerve, contributing to heart rate variability (HRV), which has been correlated with improved sleep quality. Higher HRV, reflecting the variation in time between heartbeats, is associated with a robust vagal tone. Signals from the vagus nerve play a crucial role in modulating the body's internal circadian rhythms, aiding in the synchronisation of sleep-wake cycles. Ensuring proper alignment with circadian rhythms is essential for optimising sleep quality and nighttime breathing.
Nurosym indirectly influences sleep patterns through vagus nerve stimulation. Its believed anti-inflammatory action via the vagus nerve regulates the hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis, by improving cell resilience for increased cortisol levels. As inflammation makes cells more responsive to cortisol signals, Nurosym's regulation potentially contributes to stress response reduction, aiding in preventing stress-induced insomnia.
Nurosym, known for its neuromodulatory properties, exhibits efficacy in mitigating inflammation, especially pertinent to sleep disorders. The inflammatory processes, linked to sleep disturbances, not only impact sleep but also impede nutrient absorption in the bowels. Through vagus nerve stimulation and the reduction of pro-inflammatory cytokine activity, Nurosym has the potential to establish a better environment for restful sleep, energy storage, and help to enhance memory consolidation during sleep.
Nurosym through the activation of the vagus nerve, may establish a connection to the nucleus tractus solitarii (NTS) and subsequently regulate locus coeruleus (LC) function. These brain structures are integral to sleep regulation, maintain autonomic balance, and improve overall sleep patterns.
Nurosym Research-Based Evidence
61% of Nurosym patients report a reduction in insomnia, but 83% notice an improvement in stress resilience, which in the long run may contribute to achieving proper sleep patterns.
A Parasym study, which included daily Nurosym neuromodulation sessions, showcased a trend to improve global sleep scores within a 2-week timeframe.
The group undergoing active neuromodulation experienced a 31% improvement in global sleep scores with an increased depth of sleeping, indicating more profound sleep patterns.
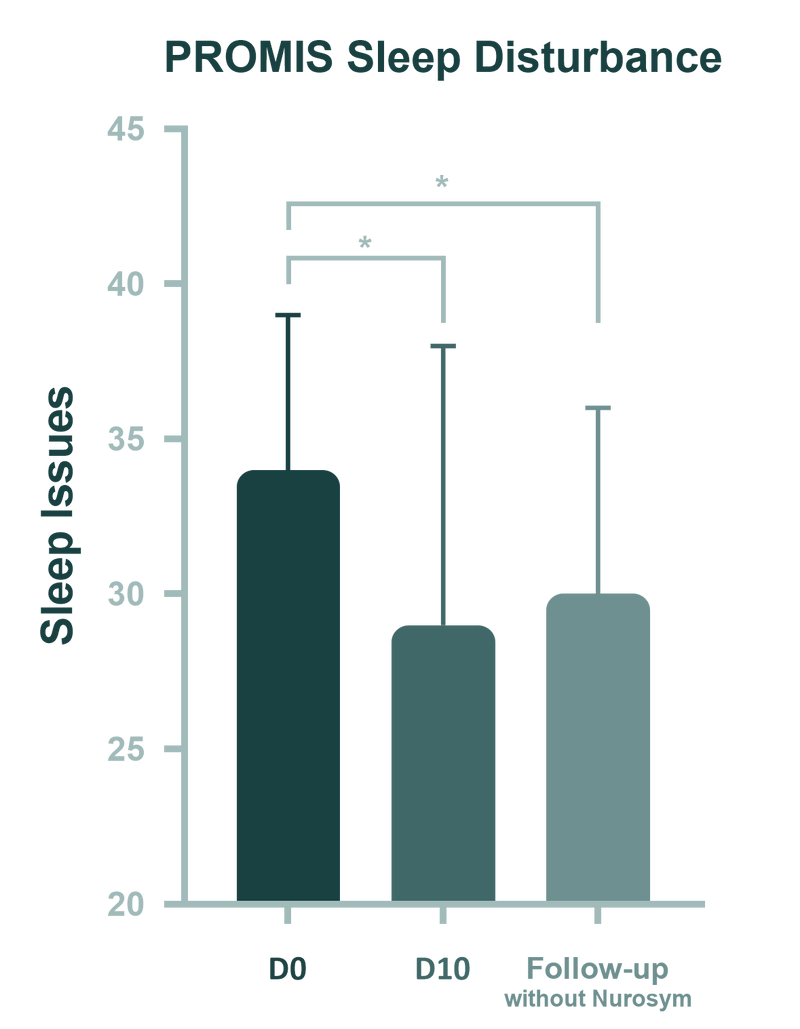
(Fig). Changes in sleep (PROMIS Sleep Disturbance) across three timepoints: pre-intervention (D0 = Day 0), post-intervention (D10 = Day 10), and 1-month follow-up. The follow-up bar, representing sleep issues without Nurosym, suggests the possibility of a carryover effect. Although Nurosym is no longer being used, the improvement in sleep issues seen by Day 10 persists at the follow-up stage. Error bars reflect standard error. *p < 0.05.
Another Parasym findings suggest a notable shift towards the parasympathetic side, indicating a more pronounced relaxation response during Nurosym neuromodulation. This was measured by a 61% improvement in heart rate variability (HF parameter), along with other HRV parameters (RMSSD, PRR50, SDRR).
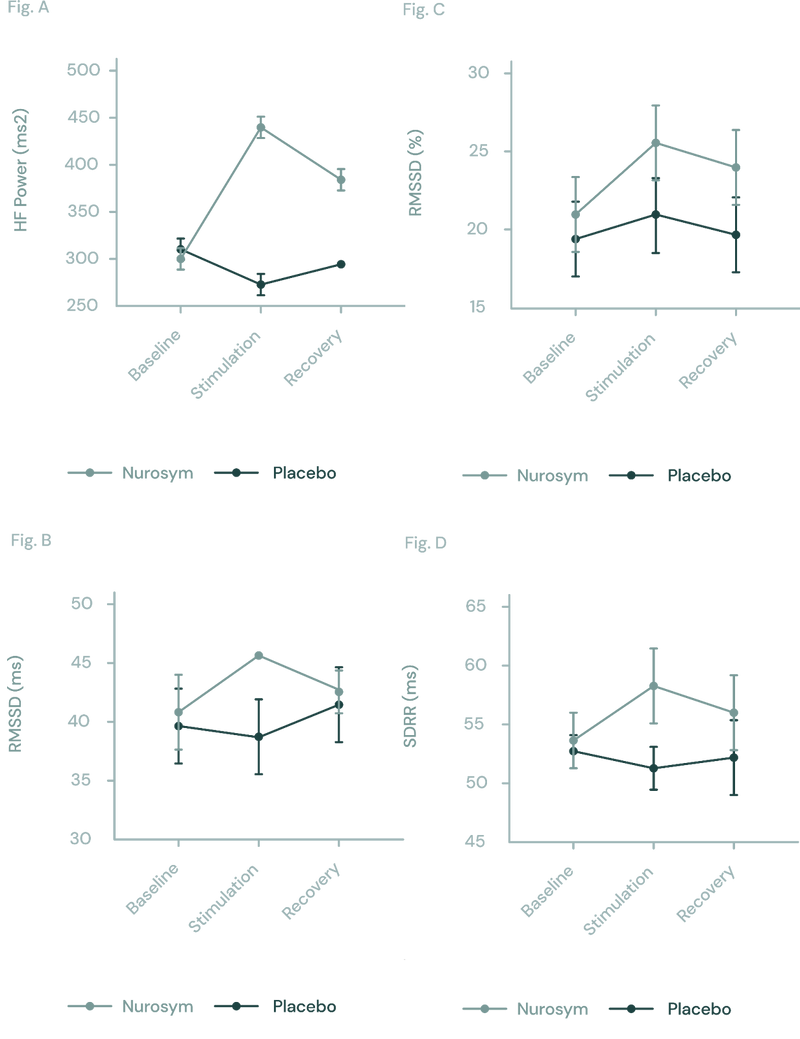
Fig (A, B, C D). The response of autonomic function measured by HRV in Nurosym or Placebo conditions over time: (A) HF, (B) RMSSD, (C) pRR50, (D) SDRR. With Nurosym, the measurements of HF, RMSSD, PRR50 and SDRR were significantly higher than those in Placebo (Parasym Clinical Trials, 2022).
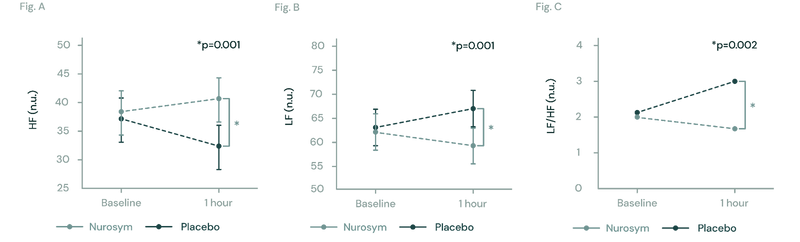
Fig (A, B, C). The figures illustrate changes in heart rate variability (HRV) during Nurosym neuromodulation. In Figure (A), High Frequency HRV significantly increases (*p=0.001). In Figure (B), Low Frequency HRV significantly decreases (*P=0. 2018).
Research has shown that pre-existing conditions like anxiety can intensify the symptoms of insomnia. The Nurosym clinical trial demonstrated a significant connection between anxiety and insomnia, revealing that a 35% reduction in anxiety symptoms was associated with notable improvements in sleep disturbances.
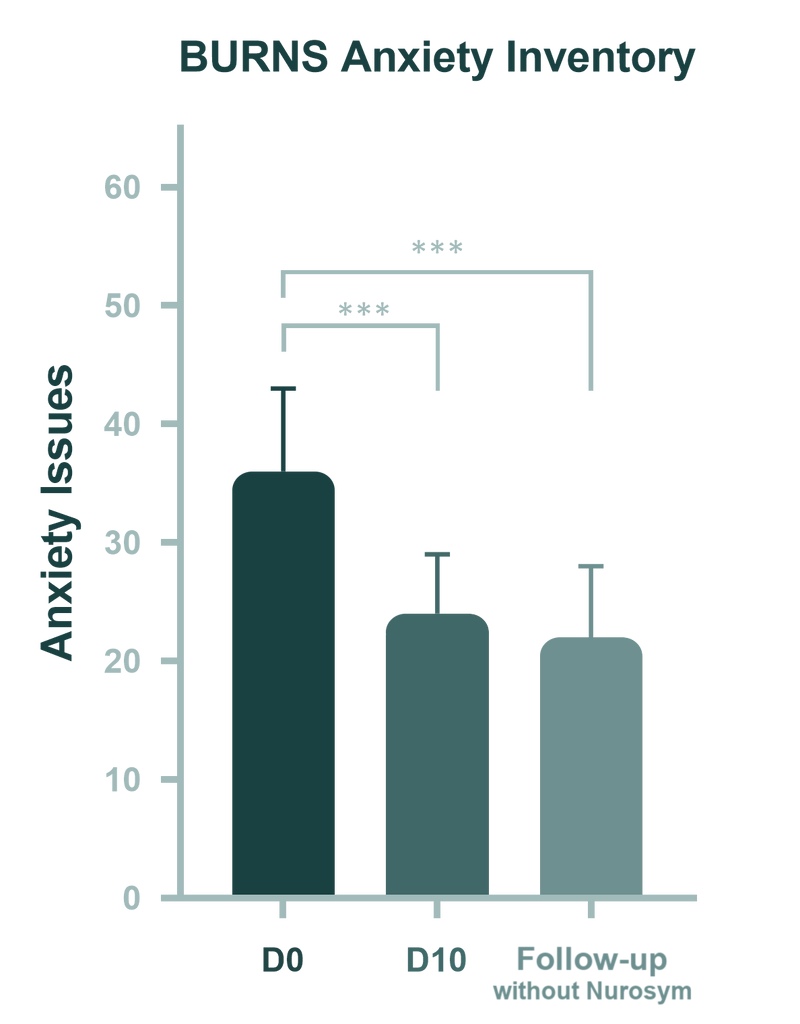
(Fig). Changes in anxiety across three timepoints: pre-intervention (D0: Day 0), post-intervention (D10: Day 10), and 1-month follow-up after accomplished treatment. Boxplots are used for nonparametric data, while column graphs depict parametric data. Error bars represent the standard error. Significant level is indicated as ***p < 0.001 (Parasym Clinical Trial, 2024).
Nurosym therapy has the potential to address sleep-related concerns in community-dwelling adults and demonstrates benign effects on sleep improvement when compared to drug treatments.
Doctors about Nurosym
Patients about Nurosym
Dawid S.
“After a week or so, I noticed a definite improvement in my mood and sleep, with that heavy feeling falling away. I’ve also used it for a neuropathic pain issue and it has helped me reduce my medication.”
Elisabeth N.
“I am able to sit up straight for longer periods without feeling faint, I fall asleep quickly and sleep more soundly, my headaches have decreased dramatically and I am able to socialise more easily.”
Who is for it?
Individuals experiencing mild to moderate insomnia, particularly those linked to mood (affective) disorders, somatic disorders, adjustment disorders arising from challenging situations, and side effects of medications, as well as other depressive and anxiety disorders. This suitability is attributed to the fact that many of these conditions stem from dysautonomia causes.
Nurosym treatment may enhance the deep sleep phase, which is often challenging to achieve with medications prescribed for insomnia. Common medications primarily address the onset of sleep, whereas Nurosym neuromodulation focuses on regeneration, restoration, and memory consolidation during the nighttime. Consequently, it proves beneficial for individuals seeking relief from addictive medication treatments, which should be used only temporarily.
Protocol - How to Use
The protocol includes a daily one-hour pre-sleep session aimed at modulating neural circuits associated with sleep-related brain structures using the Nurosym device to prevent insomnia. Using the Nurosym device before bed can help you achieve a more relaxed state, potentially help you achieve deep sleep stages while resting, and alleviate symptoms of anxiety.
Consider combining Nurostm with psychological therapy, especially if you struggle with stress-related insomnia.
If the person also struggles with anxiety disorder, consider adding an additional hour-long Nurosym session in the morning. This additional session is designed to keep your nervous system in balance throughout the day.
This device is designed specifically to address the neurobiological aspects of insomnia, offering a systematic approach to treating and alleviating insomnia symptoms through targeted parasympathetic neuromodulation interventions.
How often
Nurosym is recommended for use twice daily based on clinical research and patient feedback. This regimen ensures optimal energy balancing and nervous system calming.
How long
Users should allocate 30 minutes in the morning and 60 minutes before sleep for Nurosym therapy sessions. Consistency in application is key to achieving desired results.
Results
Positive outcomes from Nurosym therapy may become noticeable within a relatively short timeframe. Many individuals report improvements within days of starting treatment.


