Fibromyalgia and Pain and the Vagus Nerve Pathogenesis
The condition known as fibromyalgia is characterised by persistent symptoms such as widespread pain, hyperalgesia, sleep disorders, fatigue, sensations of body stiffness, a tendency towards mental disorders, and severe vegetative and functional disturbances. While the exact cause of fibromyalgia remains unknown, recent research has highlighted potential links to the vagus nerve. The aberrant vagal tone found in chronic disease states such as fibromyalgia, may be the cause and the consequence of alterations in the central nervous system. This nerve acts as a communication pathway between the brain and major bodily organs, it activates the "rest and digest" response through the parasympathetic nervous system, aiding in efficient energy conservation. However, this balance can be disrupted by excessive stress and inflammatory responses, potentially exacerbating the symptoms of fibromyalgia via (doi: 10.1016/j.neubiorev.2021.10.021):
Fight or Flight Response
According to the Nature article, fibromyalgia patients exhibit a higher heart rate and reduced heart rate variability (HRV) compared to healthy individuals. HRV, reflects the activity of the parasympathetic nervous system, which is directly regulated by the vagus nerve. Low HRV is associated with vagus nerve dysfunction, which has been observed in painful and inflammatory diseases, including fibromyalgia. Additionally, dysregulation of the autonomic nervous system may worsen pain, stress, and sleep disturbances in patients with fibromyalgia (doi: 10.1038/s41598-023-27581-9).
Neurogenic Inflammation
Impaired function of the vagus nerve can significantly contribute to neurogenic inflammation, a form of inflammation primarily mediated by the nervous system, particularly in the context of fibromyalgia. Neurogenic inflammation involves the release of neuropeptides like neuropeptide Y (NPY), leading to localised inflammatory responses. In fibromyalgia, altered vagus nerve function can disrupt the regulation of both local (neurogenic) and systemic inflammatory responses. This dysregulation may contribute to a range of symptoms commonly associated with fibromyalgia, such as insomnia, depression, anxiety, and reduced cognitive function (doi: 10.1016/j.jacep.2020.08.025, doi: 10.1016/j.neubiorev.2021.10.021).
Peripheral Inflammation & dysautonomia
The vagus nerve modulates peripheral inflammation by activating the cholinergic anti-inflammatory pathway (CAP). This pathway involves the vagus nerve transmitting inflammation signals from the body to the brainstem through the nucleus tractus solitarii (NTS) and dorsal motor nucleus, which, in turn, relays these signals to peripheral structures. This regulation is impacting immune function and hormone release throughout the body. An impaired vagus nerve cannot effectively counteract inflammation, potentially contributing to conditions in fibromyalgia characterised by excessive inflammation and other somatic symptoms such as fatigue, low-grade fever, painful lymph nodes, sore throat and migrating joint pain (doi: 10.1093/pm/pnaa164, doi: 10.1186/s42234-022-00100-3).
Changes in Neurotransmitter Systems
Fibromyalgia is often associated with dysregulation in neurotransmitters such as serotonin, norepinephrine, and acetylcholine, which interact with the vagus nerve. The vagus nerve plays a crucial role in modulating the release of neurotransmitters such as acetylcholine, norepinephrine, and serotonin. Stress-induced alterations in neurotransmitter levels may impair vagal function, while overactivity of the vagus nerve can also lead to changes in neurotransmitter production, contributing to the altered pain perception, muscle stiffness and mood disturbances often observed in fibromyalgia patients (doi: 10.1186/ar1772, doi: 10.1016/j.neubiorev.2021.10.021).
Increased Pain Sensitivity
The vagus nerve, an integral part of pain perception, influences bodily pain pathways, enabling communication between the peripheral nervous system and the central nervous system. When its function is impaired, it can result in an excessive pain response, causing increased sensitivity to stimuli that do not usually cause pain, a phenomenon known as allodynia. The vagus nerve projects to key areas of the brain such as the amygdala, hippocampus, hypothalamus, and anterior cingulate cortex, all crucial for the processing and interpretation of pain. A decrease in vagal activity can therefore disrupt normal pain perception, leading to increased sensitivity to both physical sensations and emotional responses to pain (doi: 10.1093/pm/pnaa164).
Rest and Digest Response
Nurosym boosts vagal tone, among fibromyalgia patients as evidenced by improvements in Heart Rate Variability (HRV). An increased HRV observed during Nurosym sessions signifies enhanced parasympathetic activity, or the "rest and digest '' response. Nurosym's influence on the vagal tone can positively modify respiratory patterns and reduce pain, and with a more stable autonomic nervous system can contribute to reduced stress levels and better sleep quality (doi: 10.1371/journal.pone.0263833, doi: 10.1016/j.cardfail.2022.10.278).
Mitigating Neurogenic Inflammation
Fibromyalgia often involves neurogenic inflammation. Nurosym aims to address this by specifically targeting the pathways involved in neurogenic inflammation. It works by modulating the release of neuropeptides such as neuropeptide Y (NPY) and neurotrophin (BDNF), and rebalancing the nervous system-mediated inflammatory response. This anti-inflammatory effect is associated with reduced oxidative stress markers and norepinephrine levels. Reduction in neurogenic inflammatory markers and oxidative stress are linked to improvements in neurocognitive areas, regulating emotions (amygdala), memory and learning (hippocampus), stress and hormonal responses (hypothalamus), and pain processing (anterior cingulate cortex), resulting in reduced risk of symptoms like pain, insomnia, anxiety, depression, and cognitive impairment commonly seen in fibromyalgia and related conditions (doi: 10.1161/JAHA.121.023582, 10.1016/j.cardfail.2022.10.278).
Controlling Peripheral Inflammation and Dysautonomia
Nurosym research demonstrates a decrease in systemic inflammation, a significant factor in pain perception among fibromyalgia patients. Vagus nerve activation by Nurosym aids in reducing inflammation through the cholinergic anti-inflammatory pathway (CAP), affecting both afferent and efferent fibres. Consequently, Nurosym helps control the uncontrolled release of cytokines and inflammatory molecules, inhibiting inflammatory cascades. Peripherally, it leads to reduced levels of inflammatory proteins and cytokines (like IL-6, TNF-ɑ), alleviating fibromyalgia symptoms associated with excessive inflammation, including fatigue, low-grade fever, painful lymph nodes, sore throat, and migrating joint pain (doi: 10.1161/JAHA.121.023582, doi: 10.1016/j.hrthm.2023.04.051).
Neurotransmitters Regulation
In Fibromyalgia patients, norepinephrine-evoked pain was seen in 80% individuals. Norepinephrine, a neurotransmitter associated with the body's stress response, can influence pain perception and contribute to increased pain sensitivity. Nurosym is believed to modulate neurotransmitters like serotonin, norepinephrine, and acetylcholine by promoting parasympathetic nervous system activity. Activation of the vagus nerve promotes parasympathetic dominance, which includes reducing the expression of new noradrenergic receptors. This reduction in receptor expression is associated with countering the pronociceptive effect linked to chronic stress and fibromyalgia (doi: 10.1016/j.hrthm.2023.04.051; doi: 10.3389/fpsyt.2018.00044; doi: 10.1186/1471-2474-3-2).
Reduced Pain Sensitivity
Nurosym has demonstrated efficacy in reducing pain responses by modulating peripheral and central nociceptive functions through increased vagal tone. Increased vagal tone is associated with decreased pain sensitivity and stress responses. This modulation improves communication between peripheral and central nervous systems, including cortical and subcortical areas. As a result, Nurosym reduces pain-induced neuronal activation, particularly in the caudal trigeminal nucleus, leading to a reduction in pain symptoms and trigeminal allodynia. Restoration of vagal activity may lead to decreased sensitivity to both physical sensations and emotional responses to pain (doi: 10.1093/pm/pnaa164).
Nurosym Research-Based Evidence
71% of patients using Nurosym reported a decrease in chronic somatic pains, leading to mood improvement and a reduction in future-related complications in fibromyalgia and pain-related conditions within just 2 weeks. The reported decrease in pain was correlated with a diminishing of painful lymph nodes, sore throat, and migrating joint pain.
Moreover, 83% of patients using Nurosym reported a decrease in fibromyalgia symptoms, chronic fatigue syndrome, depression, gastrointestinal problems, stress, and low-grade fever.
Reduced HRV is associated with autonomic dysregulation and increased pain perception. Patients using Nurosym observed HRV enhancements and the research has indicated 61% improvement (doi: 10.1371/journal.pone.0263833).
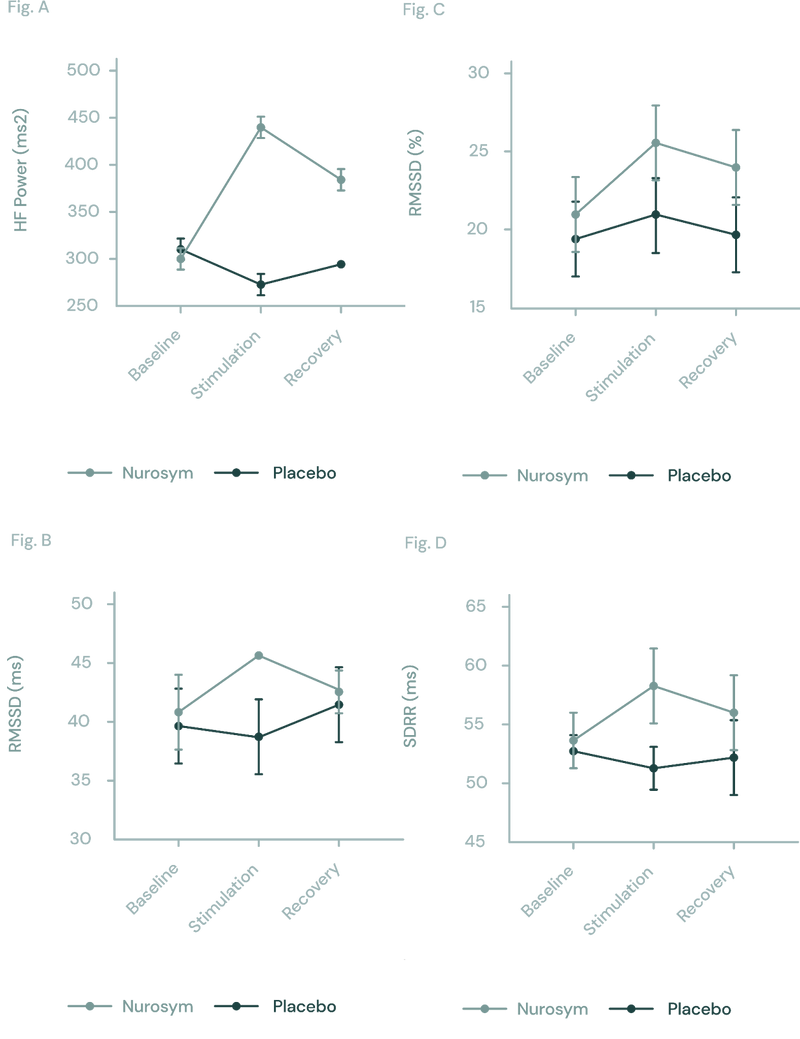
Fig (A, B, C D). The response of autonomic function measured by HRV in Nurosym or Placebo conditions over time: (A) HF, (B) RMSSD, (C) pRR50, (D) SDRR. With Nurosym, the measurements of HF, RMSSD, PRR50 and SDRR were significantly higher than those in Placebo (Parasym Clinical Trials, doi: 10.1371/journal.pone.0263833).
Another Nurosym finding highlights significant remission of debilitating symptoms, particularly the alleviation of brain fog, widespread pain, headaches, depression and fatigue in all dysautonomia patients enrolled in the investigation by 40% (doi: 10.51956/ANNR.100011).
After 2 weeks of Nurosym neuromodulationtherapy, patients experienced an average of 57% improvement in widespread pain and profile of mood states related to ME/CFS as evidenced in Parasym clinical trials. Before therapy, patients had significant problems related to extensive pain, with an intensity of at least 3 on the symptom severity scale from 0 to 5 in the study. Additionally, in a previous study conducted by Dr Benjamin Natelson directly indicated the implications of a significant reduction in pain for fibromyalgia (FM) patients through vagus nerve stimulation (doi: 10.1101/2022.11.08.22281807).
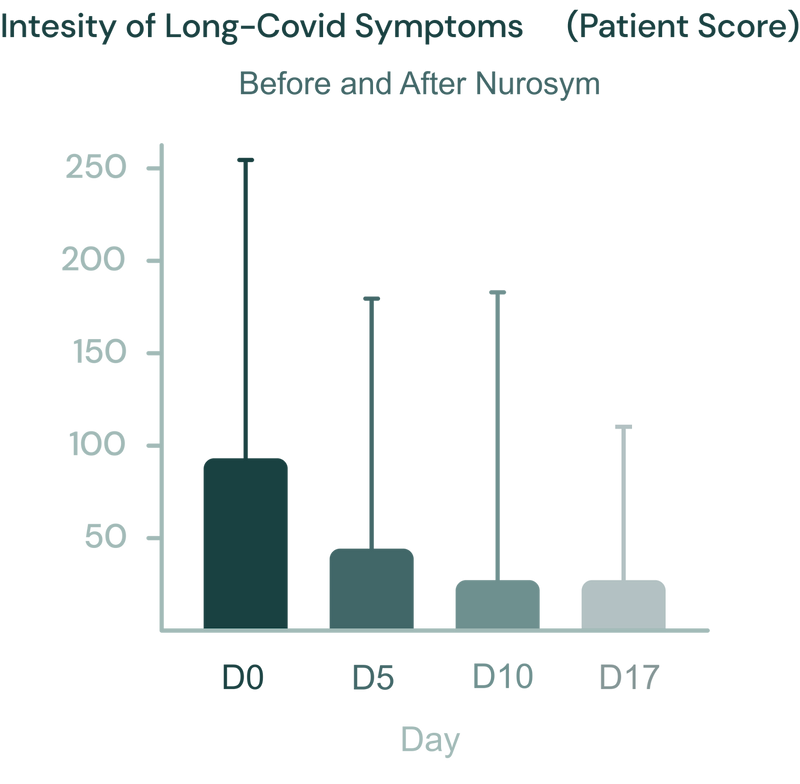
Fig. Evolution of the severity of the syndrome, during treatment (day 0, day 5, day 10), and 1 week after ending Nurosym neuromodulation (follow-up). The individual values and the median are shown. Non parametric Friedman statistics for paired comparisons were used and followed by post-hoc Dunn’s multiple comparisons test (Parasym Clinical Trials, doi: 10.51956/ANNR.100011).
During Parasym trials, reduction of 45% on the Beck Depression score was observed, directly correlating with mood improvement (doi: 10.51956/ANNR.100011).
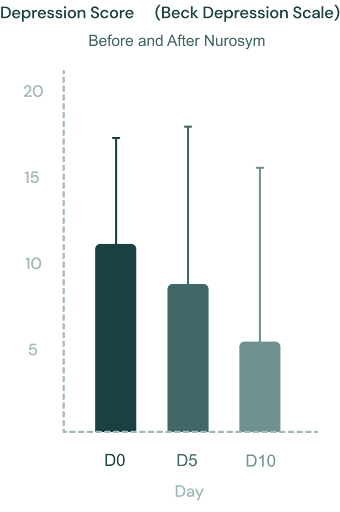
Fig. Evolution of the Beck depression scale scores during Nurosym treatment (day 0, day 5 and day 10). The individual values and the median are shown. Non parametric Friedman statistics for paired comparisons were used and followed by post-hoc Dunn’s multiple comparisons test. (doi: 10.51956/ANNR.100011).
48% fatigue improvement was evident in the research findings, reflecting positive energy outcomes on patients (doi: 10.51956/ANNR.100011).
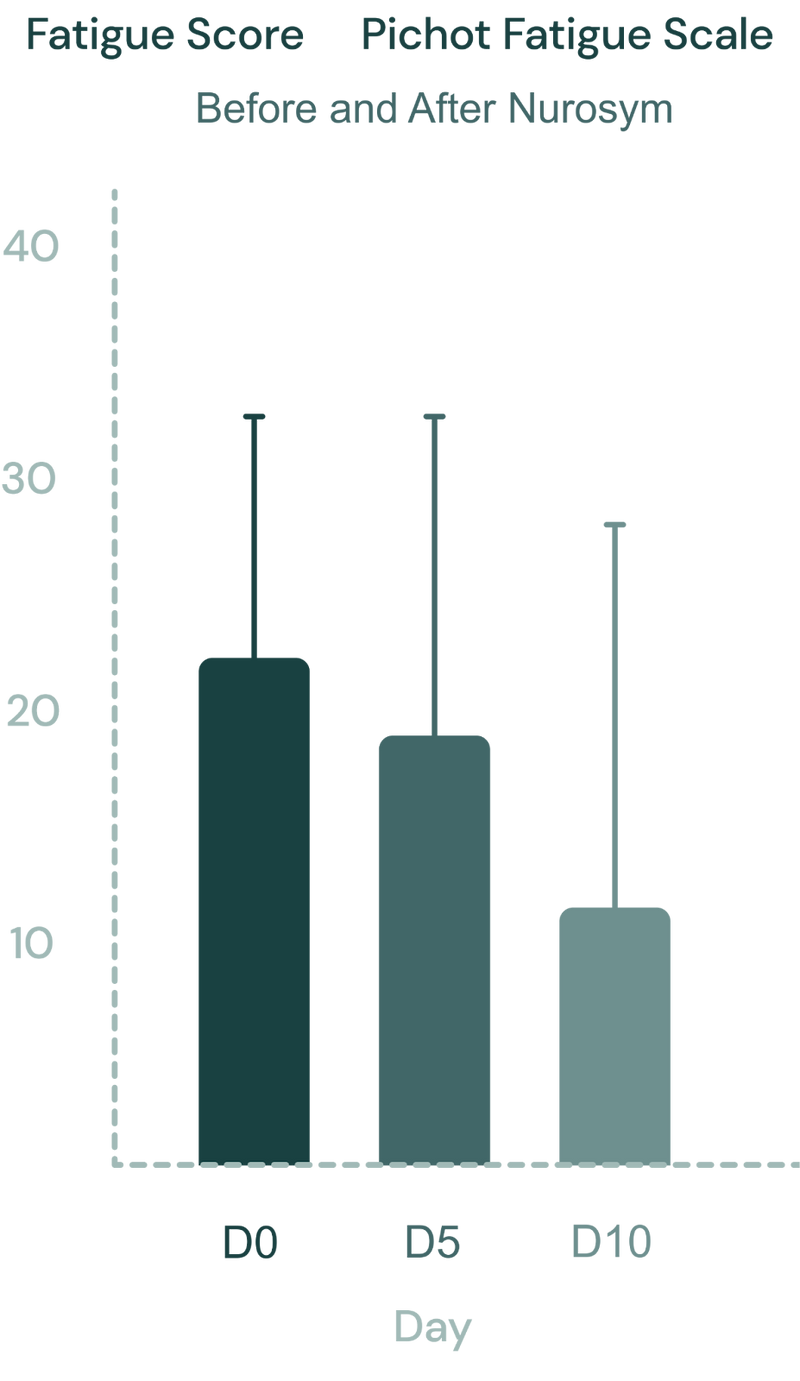
Fig. The Pichot fatigue scale scores during Nurosym therapy (D0: day 0, D5: day 5 and D10: day 10). Significant improvement in fatigue scores after Nurosym treatment was observed (D0 vs. D10, p<0.0001). (Parasym clinical trial, doi: 10.51956/ANNR.100011).
Another Nurosym finding highlights 78% reduction in inflammation (cytokines levels like IL-8, Il-6, TNF-α). This reduction in inflammation is correlated with a decrease in pain perception and an improvement in gastrointestinal function (doi: 10.1016/j.cardfail.2022.10.278).
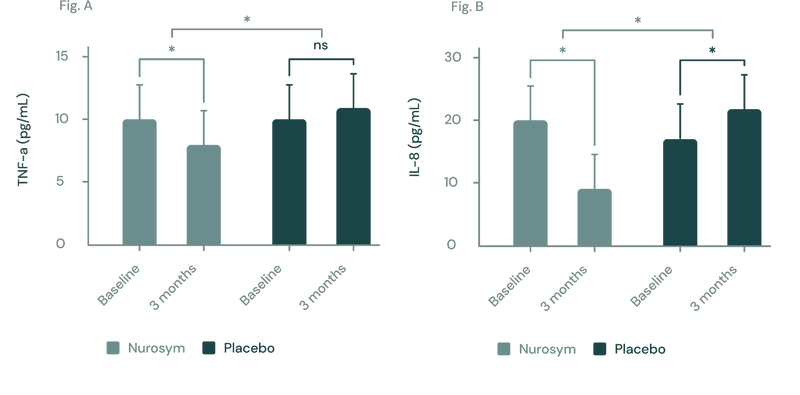
Fig. (A, B) In a three-month study employing the Nurosym device for heart failure patients, notable improvements (*P<0.05) were noted in inflammatory biomarkers: (A) Tumor Necrosis Factor (TNF)‐α exhibited a ~23% reduction, while (B) Interleukin (IL)‐8 showed a marked ~61.3% reduction. The investigation specifically targeted participants with elevated baseline inflammation levels (doi: 10.1016/j.cardfail.2022.10.278).
Fibromyalgia can correlate with cognitive impairment due to persistent fatigue. In clinical trials conducted by Parasym, individuals exhibited an improvement within 5 days, showing a 32% enhancement in memory and a 26% boost in learning performance with the use of Nurosym (doi: 10.1016/j.brs.2020.10.012).
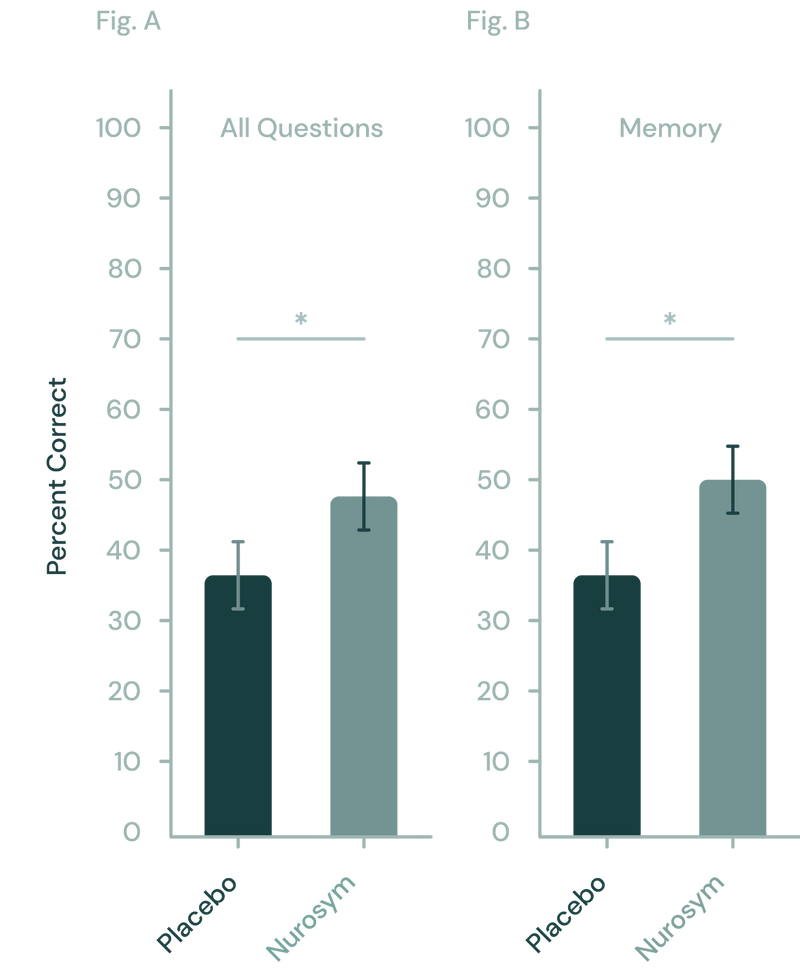
Fig (A, B). Nurosym has shown to enhance memory in learning tasks relative to a placebo. (A) Across all test questions, Nurosym's neuromodulation demonstrated a notable advantage over placebo. (B) Specifically, this improvement was largely due to the significant impact of Nurosym neuromodulation on memory-related questions (Parasym Clinical Trials, doi: 10.1016/j.brs.2020.10.012).
Doctors about Nurosym
Patients about Nurosym
David
“I was worried that Parasym wouldn’t make any difference when I first used it, but I was wrong. After a week or so, I noticed a definite improvement in my mood and sleep, with that heavy feeling falling away. I’ve also used it for a neuropathic pain issue and it has helped me reduce my medication. It’s now a part of my regular routine, and I wouldn’t be without it”
“I have endometriosis, and along with the chronic pain and other debilitating symptoms, I also frequently suffer from fatigue and brain fog. And I had heard that this device might be helpful in mitigating those. So it arrived and I found that it did really, really help particularly my fatigue and my brain fog. But it also seemed to help my pain. I had fewer pain days. I track them quite religiously and I was, it was, I wasn't expecting the device to really help with the pain (...)So yes, I've had a very good experience with it, and I'd recommend it to anybody who was hoping for relief, particularly from fatigue and brain fog symptoms”.
“I’ve struggled with Lyme disease, autonomic issues, EBV, pituitary problems including adrenal insufficiency, fatigue, insomnia and gastrointestinal issues. It was very serious, in and out of hospitals, I needed a wheelchair and was practically bed bound for several years. Many days I couldn’t even lift my head off the pillow due to my fatigue and Postural tachycardia syndrome (PoTS). I’ve seen so many doctors and taken so many different medications and supplements. With the Parasym I now have a tool I can use myself at home which doesn’t have the nasty side effects medications do. My PoTS, although still present, is much more manageable”.
Who is for it?
In the management of fibromyalgia, emphasis is placed on non-pharmacological approaches, making Nurosym a fitting therapy for individuals grappling with these conditions. Transcranial vagus nerve stimulation stands out as a non-invasive neuromodulation technique within this context, demonstrating notable efficacy in addressing fatigue, low-grade fever, joint and muscle pain, and symptoms resembling mild myopathy or arthritis, including those akin to rheumatoid arthritis (RA).
Nurosym exhibits effectiveness in reducing pain and has antidepressant potential, obviating the need for potent painkillers and psychotropic medications with substantial side effects and the somatic symptoms seen in fibromyalgia. While antiepileptic drugs are commonly employed in fibromyalgia treatment, it's worth noting that vagus nerve stimulation is an FDA-approved method for refractory epilepsy treatment. Consequently, Nurosym emerges as a multi-faceted therapeutic approach that could potentially replace multiple medications, offering a more streamlined strategy for individuals dealing with fibromyalgia and extensive pain.
Protocol - How to Use
Based on research results and patient feedback, it is recommended that Nurosym sessions be administered for the treatment of fibromyalgia and related syndromes for at least 30 minutes twice daily – preferably in the morning and at bedtime – to enhance the central nervous system's response to pain perception, potentially facilitating better sleep and aiding in overall symptom alleviation.
However, the Nurosym protocol can be tailored to the individual's reaction and needs by adjusting the intensity to the patient. It has been shown that a higher intensity of therapy can reduce inflammatory processes, which may additionally affect the perception of pain. Although some people may experience improvement in as little as 5 days, particularly in terms of reducing fatigue, optimal results are usually achieved after a four-week treatment period. Continuing therapy beyond this time is advisable to maintain stress resilience.
How often
Nurosym is recommended for use twice daily based on clinical research and patient feedback. This regimen ensures optimal energy balancing and nervous system calming.
How long
Users should allocate 30 minutes in the morning and 60 minutes before sleep for Nurosym therapy sessions. Consistency in application is key to achieving desired results.
Results
Positive outcomes from Nurosym therapy may become noticeable within a relatively short timeframe. Many individuals report improvements within days of starting treatment.


